
Retiree Dental Plans
Member Guidebook
Pensions & Benefits
HD-0714-0124
The Dental Plan Organizations and The Dental Expense Plan
For Retired Group Members of the State Health Benets Program and School Employees’ Health Benets Program
Retiree Dental Plans — Member Guidebook January 2024 Page 2
State Health Benets Program School Employees’ Health Benets Program
TABLE OF CONTENTS
Introduction ...............................3
Retiree Dental Plans Eligibility ................3
Eligible Retirees ...........................3
COBRA Members .........................3
Waiver of Enrollment for
Other Dental Coverage .....................4
Eligible Dependents ........................4
Enrolling in the Retiree Dental Plans. . . . . . . . . . . 4
How to Enroll .............................4
Enrolling Dependents ......................4
Levels of Coverage ........................4
Dual Dental Plan Enrollment is Prohibited. . . . . . . 4
Retiree Dental Plan Premiums ...............5
When Coverage Begins. . . . . . . . . . . . . . . . . . . . . 5
End of Coverage ..........................5
Survivor Coverage .........................5
Extension of Coverage Provisions ............5
If Eligibility Ends While
Undergoing Treatment ......................6
For Children Over the
Age of 26 With Disabilities ...................6
Coordination of Benets With
Other Insurance Plans ......................6
Retiree Dental Plan Organizations .............6
Considerations When Choosing a DPO ........7
Retiree DPO Reimbursement Tiers ............7
Covered Services ..........................8
More Expensive Services ..................17
Emergency Services — Out of Area ..........17
Services Not Covered by the DPO ............17
Retiree Dental Expense Plan ................17
Deductibles .............................17
Discounted Fee-for-Service Network .........17
Reasonable and Customary Allowance .......18
Reimbursement ..........................18
Annual Benet Maximum ..................18
Plan Design ..............................18
Three Tier Benet Design. . . . . . . . . . . . . . . . . 18
Covered Services .........................18
Preventive Care ..........................18
Basic Services ...........................18
Retiree Dental Expense Plan
Reimbursement Tiers (Chart) ................19
Major Restorative Services .................19
Additional Provisions of the Plan ............19
How Payments Are Made ..................19
Filing Deadline ...........................20
Itemized Bills ............................20
Predetermination of Benets ................20
Alternative Procedures ....................20
DEP Services
Eligible For Reimbursement ................20
DEP Services Not
Eligible For Reimbursement .................21
Appendix I ...............................22
Claim Appeal Procedures ...................22
HIPAA Privacy ............................22
Audit of Dependent Coverage ...............22
Health Care Fraud .........................22
Appendix II ...............................23
Glossary .................................23
Appendix III ..............................23
Notice of Privacy Practices to Enrollees ......23
Protected Health Information ...............23
Uses and Disclosures of PHI ...............24
Restricted Uses .........................24
Member Rights ..........................24
Questions and Concerns ..................25
Appendix IV ..............................26
Participating Retiree Dental Plans ............26
Health Benets Contact Information ..........27
Addresses ..............................27
Telephone Numbers ......................27
Health Benet Publications .................27
General Publications. . . . . . . . . . . . . . . . . . . . . . 27
Health Benet Fact Sheets .................27
Health Plan Member Guidebooks ............27
Page 3 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
INTRODUCTION
The State Health Benets Program (SHBP) was es-
tablished in 1961. It oers medical, prescription drug,
and dental coverage to qualied State and local gov-
ernment public employees, retirees, and eligible de-
pendents. Local employers must adopt a resolution to
participate in the SHBP.
The State Health Benets Commission (SHBC) is
the executive organization responsible for overseeing
the SHBP.
The State Health Benets Program Act is found in the
New Jersey Statutes Annotated, Title 52, Article 14-
17.25 et seq. Rules governing the operation and admin-
istration of the program are found in Title 17, Chapter 9
of the New Jersey Administrative Code.
The School Employees’ Health Benets Program
(SEHBP) was established in 2007. It oers medical,
prescription drug, and dental coverage to qualied lo-
cal education public employees, retirees, and eligible
dependents. Local education employers must adopt a
resolution to participate in the SEHBP.
The School Employees’ Health Benets Commis-
sion (SEHBC) is the executive organization responsi-
ble for overseeing the SEHBP.
The School Employees’ Health Benets Program Act is
found in the New Jersey Statutes Annotated, Title 52,
Article 14-17.46 et seq. Rules governing the operation
and administration of the program are found in Title 17,
Chapter 9 of the New Jersey Administrative Code.
The New Jersey Division of Pensions & Benets
(NJDPB), specically the Health Benets Bureau and
the Bureau of Policy and Planning, are responsible for
the daily administrative activities of the SHBP and the
SEHBP.
The Retiree Dental Plans are available to retirees eli-
gible for enrollment in the SHBP or the SEHBP. Before
making any enrollment decision, you should carefully
review the standards of eligibility and the conditions,
limitations, and exclusions of the coverage oered un-
der the plans.
Every eort has been made to ensure the accuracy of
the Retiree Dental Plans Member Guidebook; howev-
er, State law and the New Jersey Administrative Code
govern the SHBP and SEHBP. If there are discrepan-
cies between the information presented in this guide-
book and/or plan documents and the law, regulations,
or contracts, the law, regulations, and contracts will
govern. Furthermore, if you are unsure whether a den-
tal service or procedure is covered, contact your dental
plan before you receive services to avoid any denial of
coverage issues that could result.
If, after reading this guidebook, you have any ques-
tions, comments, or suggestions regarding the infor-
mation presented, please write to the New Jersey Di-
vision of Pensions & Benets, P.O. Box 295, Trenton,
NJ 08625-0295, call (609) 292-7524, or send email to:
pensions.nj@treas.nj.gov
RETIREE DENTAL PLANS ELIGIBILITY
Eligible Retirees
Enrollment in the Retiree Dental Plans is voluntary.
You have one opportunity to enroll in a Retiree Dental
Plan when you rst become eligible for Retired Group
SHBP or SEHBP health plan coverage. A retiree must
submit a SHBP/SEHBP Retiree Dental Plan Appli-
cation online through Benetsolver within 60 days of
retirement or when rst eligible for enrollment or lose
the ability to enroll (except as specically stated in the
“Waiver of Enrollment for Other Dental Coverage” sec-
tion). Benetsolver can be accessed by navigating to
mynjbenetshub or by logging into your myNewJersey
account.
The Retiree Dental Plans are available to the following:
• Any retiree, including surviving eligible depen-
dents, enrolled in a health plan in the Retired
Group of the SHBP or SEHBP.
• Eligible retirees, including surviving eligible de-
pendents, who elect to waive medical coverage
because of other SHBP or SEHBP coverage or
group coverage provided from another employer,
either as a dependent of a spouse, or partner, or
through their own employment.
COBRA Members
If at retirement you are eligible to enroll for coverage
in the Retired Group of the SHBP or SEHBP, you can-
not continue employee dental plan coverage under the
Consolidated Omnibus Budget Reconciliation Act of
1985 (COBRA). You must choose to enroll in a Retiree
Dental Plan within 60 days of retirement or when rst
eligible if waived for other coverage or you will lose the
ability to enroll under Retiree Dental Plan coverage.
Retiree Dental Plans — Member Guidebook January 2024 Page 4
State Health Benets Program School Employees’ Health Benets Program
Waiver Of Enrollment
For Other Dental Coverage
The one-time dental plan enrollment opportunity can
be deferred if an otherwise eligible individual has
other group dental coverage, either as a dependent
of a spouse, civil union partner, or domestic partner,
through their own employment under an employer plan,
or through an eligible retiree group association. An eli-
gible retiree group association is an association whose
membership is limited based on the former employ-
ment of the retiree or retiree’s dependent.
A retiree or eligible survivor may elect to waive enroll-
ment at the time of retirement or rst oering and retain
the right to enroll at a later date. The individual must
enroll online through Benetsolver within 60 days of the
loss of the other group dental coverage.
Proof of the other group dental plan termination of cov-
erage must be submitted online through Benetsolver
in the form of a HIPAA Certication of Coverage form
or a letter from the employer.
Eligible Dependents
Your eligible dependents are your spouse, civil union
partner, or eligible same-sex domestic partner and/or
your eligible children.
For denitions of eligible dependents and more infor-
mation about supporting documentation, visit our web-
site at: www.nj.gov/treasury/pensions
Note: Extended coverage provisions under P.L. 2005,
c. 375 (Chapter 375), for certain over age children
and the extension of coverage under the provisions of
federal COBRA law do not apply to the Retiree Dental
Plans. When Retiree Dental Plans coverage ends for
yourself or your dependents, there are no other provi-
sions for extending coverage.
ENROLLING IN THE RETIREE DENTAL PLANS
How to Enroll
For new retirees or individuals becoming eligible for
Retired Group SHBP or SEHBP coverage, the NJDPB
will include dental enrollment materials at the same
time it sends the Retired Group health plan oering,
which is generally within 30 to 60 days of retirement or
eligibility for retiree group plan coverage. The election
of dental coverage must be completed online through
Benetsolver by navigating to mynjbenetshub or via
your myNewJersey account.
If you are covered under a group dental plan as a de-
pendent or as an employee through other employment
when rst oered enrollment, you may opt to waive the
Retiree Dental Plans and elect to enroll at a future date
if your other coverage has ended. To waive coverage,
you must do so online through Benetsolver. To enroll
at a later date, you must submit an online application
through Benetsolver within 60 days of the loss of the
other dental coverage. Proof of loss of coverage must
be submitted with the online enrollment application.
Acceptable documentation includes a letter from the
employer providing date of termination of coverage, a
HIPAA Certication of Coverage form, etc.
Enrolling Dependents
You may enroll your eligible dependents when you en-
roll.
If you have a new dependent, you may enroll the de-
pendent eective the date you acquired the dependent,
provided you submit an online application through Ben-
etsolver within 60 days of the dependent’s eligibility.
If you do not enroll an eligible dependent because of
other coverage and that coverage is lost, you can enroll
that dependent providing you submit an online appli-
cation through Benetsolver within 60 days of the the
loss of coverage. A copy of your dependent’s HIPAA
Certication of Coverage form must be submitted with
the online enrollment application. Coverage for that de-
pendent will be eective the date of the qualifying event
(date of loss of other coverage).
If you do not enroll a dependent within 60 days of eligi-
bility, there will be at least a two-month waiting period
from the date the online enrollment is submitted until
the dependent is covered. Coverage for that dependent
will be eective the rst day of the month following a
minimum 60-day waiting period. A dependent added in
this manner may be added to a retiree’s contract only
once.
Levels of Coverage
There are four levels of coverage oered through the
plan:
• Single: covers the retiree only.
• Member (Retiree) and Spouse/Partner: covers
the retiree and a spouse, civil union partner, or eli-
gible same-sex domestic partner.
• Parent and Child(ren): covers the retiree and all
enrolled eligible children.
• Family: covers retiree, spouse/partner, and all en-
rolled eligible children.
Dual Dental Plan Enrollment is Prohibited
You and your spouse/partner may be covered under a
dental plan as an SHBP or SEHBP eligible employee/
retiree or as a dependent, but not as both. For example,
if two retirees are married to each other and both are
eligible for SHBP and/or SEHBP enrollment, each may
elect to enroll for single coverage only, or one retiree
may enroll the other as a dependent if the other person
waives dental plan coverage. Furthermore, two em-
ployees/retirees cannot each enroll the same children
as dependents under their respective dental coverage.
Page 5 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
Retiree Dental Plans Premiums
Most retirees will pay the full cost of the Retiree Dental
Plans. The State does not pay for the cost of coverage.
However, under certain circumstances, a local public
employer that participates in the SHBP or SEHBP may
elect to pay for or share the cost of coverage for its re-
tirees under P.L. 1999, c. 48 (Chapter 48).*
Premium payments are deducted from your monthly
pension check. If your monthly pension check amount
is not sucient to cover the full premium, you will be
billed monthly in advance of the coverage period.
You will also be billed directly for coverage if you re-
ceive a pension not paid by the NJDPB, i.e., the Alter-
nate Benet Program (ABP).
*Chapter 48 allows some local employers to pay all or
a portion of the premium cost of the plan for eligible re-
tirees as a result of collective negotiation agreements.
To do this, an eligible employer must le a Chapter 48
Resolution pertaining to the Retiree Dental Plans with
the Health Benets Bureau of the NJDPB. These provi-
sions would not apply to any local retiree who receives
retiree health coverage at State (as opposed to local
employer) expense.
When Coverage Begins
Coverage under a Retiree Dental Plan will become
eective the same date as your Retired Group health
plan coverage, provided that coverage is elected online
through Benetsolver.
• The eective date of coverage for a retiree (and
eligible dependents) who was covered for health
coverage as an active employee in the SHBP or
SEHBP is approximately one month after the date
of retirement, and generally coincides with the date
that coverage as an active employee is terminated.
• The eective date of coverage for a new retiree
(and eligible dependents) who was not covered as
an active employee in the SHBP or SEHBP is the
date of retirement.
• The eective date of coverage for members who
retire from a board of education, vocational/techni-
cal school, or special services commission, partic-
ipate in their employer’s health plan (not SEHBP)
and enroll in the SEHBP Retired Group when they
enroll in Medicare, will be the date that their Medi-
care Parts A and B are eective.
• The eective date of coverage for a surviving
spouse or partner and eligible children is the date
the coverage terminates as a dependent due to the
death of the retiree.
End of Coverage
Your coverage under a Retiree Dental Plan terminates
if:
• You formally request termination in writing, or by
canceling your coverage online through Benet-
solver;
• Your retirement is canceled;
• Your pension allowance is suspended;
• You do not pay your required premiums;
• Your former employer withdraws from the SHBP
and/or SEHBP (this may not apply to certain retir-
ees of education, police, and re employers);
• Your Medicare coverage ends;
• You die (see the “Survivor Coverage” section);
• The SHBP and/or SEHBP is discontinued; or
• You become ineligible for Retired Group medical
coverage through the SHBP or SEHBP.
Coverage for your dependents will end if:
• Your coverage ceases for any of the reasons previ-
ously listed;
• Your dependent is no longer eligible for coverage
(divorce of a spouse; dissolution of a civil union or
same-sex domestic partnership; child turns age 26
unless the dependent child qualies for continu-
ance of coverage due to disability);
• Your enrolled dependent enters the Armed Forces;
or
• Your dependents becomes enrolled on their own
through the SHBP or SEHBP in a dental plan as a
subscriber.
In general, once Retiree Dental Plans coverage is ter-
minated it will not be reinstated.
Survivor Coverage
If you, the retired member, predecease your covered
dependents, your surviving dependents may be eligible
for continued coverage in a Retiree Dental Plan. Sur-
viving dependents are generally notied of their rights
to continued coverage at the time the NJDPB is notied
of the death of the retiree; however, they may contact
the NJDPB Oce of Client Services for enrollment in-
structions or for more information. It is imperative that
survivors notify the NJDPB as soon as possible after
your death because their dependent coverage termi-
nates the 1st of the month following the date of your
death.
EXTENSION OF COVERAGE PROVISIONS
Once coverage is terminated for you or any of your de-
pendents, there is no eligibility for continuation of the
Retiree Dental Plans under the provisions of COBRA.
There is no conversion to an individual policy autho-
Retiree Dental Plans — Member Guidebook January 2024 Page 6
State Health Benets Program School Employees’ Health Benets Program
rized under this plan.
If Eligibility Ends While Undergoing Treatment
If your coverage is terminated due to your voluntary
termination from the plan or failure to pay the required
premium, there is no extension of ongoing treatment for
you or your dependents.
If you die, and your dependents do not elect to continue
Retiree Dental Plans coverage under their own account
and are undergoing treatment, coverage will be extend-
ed to cover the following procedures for up to 30 days
following the end of their coverage:
• Production of an appliance or modication of an
appliance for which the impression was taken
while the person was covered;
• Preparation of a crown or restoration for which a
tooth was prepared while the person was covered;
or
• Root canal therapy for which the pulp chamber
was opened while the person was covered.
For Children Over the Age of 26 With Disabilities
In certain circumstances, coverage can be contin-
ued for a dependent child over the age of 26. See the
NJDPB website at: www.nj.gov/treasury/pensions
for more information about extending coverage for chil-
dren with disabilities.
COORDINATION OF BENEFITS
WITH OTHER INSURANCE PLANS
There is no coordination of benets between two
SHBP/SEHBP dental plans because no member is el-
igible for coverage under more than one dental plan.
You and your spouse/partner may be covered under a
dental plan as an employee/retiree or as a dependent
but not as both.
If you and your dependents are covered under a den-
tal plan other than through the SHBP/SEHBP, certain
rules apply that determine which plan provides the pri-
mary coverage and how much each plan will reimburse
you. The purpose of these rules is to prevent a com-
bined reimbursement from both plans that exceeds the
expenses that you actually incur. Although there may
be special cases not described here, the basic deter-
mination of which plan provides primary coverage is as
follows:
• The retiree’s primary dental coverage is provided
by the Retiree Dental Plans. If the retiree is also
employed, and has dental coverage through an-
other employer other than the State, then the den-
tal coverage provided by the employer is primary
to the Retiree Dental Plans.
• If your spouse/partner is enrolled as your depen-
dent and is also covered by a dental plan through
his or her employer, your spouse/partner’s prima-
ry coverage and any dependents also covered by
your spouse/partner is through the dental plan of-
fered by his or her employer.
• Coverage through a parent’s active employment is
primary over coverage through a retiree for chil-
dren.
• If your children are enrolled as dependents in your
plan and your spouse/partner’s plan, their primary
coverage is provided by the dental plan of the par-
ent whose birthday falls earlier in the year. If your
spouse/partner’s plan does not follow this rule,
then the rule in the other plan will determine the
order of benets.
• In the case of a separation or divorce, the primary
coverage for a child is provided in this order: by
the plan of the parent who is legally responsible for
the dental expenses of the child; by the plan of the
parent with custody of the child; by the plan of the
spouse/partner of the parent with custody of the
child; or by the plan of the non-custodial parent.
THE RETIREE DENTAL PLAN ORGANIZA-
TIONS
A Dental Plan Organization (DPO) is similar to a medi-
cal Health Maintenance Organization (HMO) program.
The full cost for most services is prepaid to your dentist,
but certain services require an additional copayment
from you. Also, if you choose a more expensive treat-
ment than deemed appropriate by your dental provider,
you must pay the extra cost. Further, you will not be
covered for services if you go to a dentist who is not a
member of your DPO, unless you are referred by your
DPO dentist. There are several DPOs included among
the Retiree Dental Plan. Among these organizations,
there are two types of plans – Dental Center and Indi-
vidual Practice Associations (IPA).
• Dental Centers employ a group of dentists and
technicians who are located at a central oce. In a
Dental Center Plan, you do not have the option to
select a particular dentist unless permitted by the
Dental Center. However, some DPOs oer both a
Dental Center and a list of participating dentists,
thereby giving you the option of selecting a center
or a particular dentist.
• Individual Practice Associations (IPA) consists
of a network of participating dentists who work in
their own oces. If you choose an IPA, you must
select a specic dentist in the IPA who will treat
you and your dependents.
The DPO dentist is responsible for providing all of the
services that are listed as covered in this guidebook.
If the participating dentist that you have selected does
not provide a specic service, then the DPO must refer
you to another participating dentist located within 10
Page 7 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
miles of your dentist’s oce. If you agree, the DPO may
also refer you to a dentist located beyond these limits.
If the DPO has no participating dentist who can provide
the service in your geographical area, the DPO must
refer you to a nonparticipating dentist within the 10- or
20-mile limit. If there is no dentist within this area, you
must be referred to the dentist closest to your dentist’s
oce.
If the DPO dentist refers you to another dentist and that
referral is approved by the DPO, you will have the same
coverage for the service as if you had been treated by
your dentist. However, if you select an outside dentist
on your own, the service will not be covered.
CONSIDERATIONS IN CHOOSING A DPO
• Obtain a list of DPOs and participating dentists
from your benets administrator. If you choose a
dentist rather than a Dental Center, check with the
DPO and the dentist to be sure that the dentist is
a member of the DPO, services members of the
Retiree Dental Plans, and will accept you as a new
patient.
• If you choose a dentist, you should also check with
the dentist to make sure that they plan to stay in the
DPO. If the dentist leaves, you will have to select
another dentist who participates with that DPO.
• You should also check to determine that the DPO
dentist or center can serve the needs of your entire
family and whether the days and hours of opera-
tion are convenient for you and your family.
• If your dentist leaves the DPO, and there are no
other dentists in the DPO within 30 miles of your
home, you may switch to another dental plan (ei-
ther another DPO or the Dental Expense Plan
(DEP)).
Retiree DPO Reimbursement Tiers
It is important for plan members to go for regular dental
checkups, not only for their own health, but also be-
cause treatment in later years could be more expen-
sive for them if they do not. To protect the plans and
enrolled members against the eect of retirees joining
who have gone years without any dental treatment, the
plans have three benet tiers — Tiers 1, 2, and 3. If you
enroll in a Retiree Dental Plan within 60 days of leaving
another group dental program in which you were en-
rolled for a minimum of 12 months, you will be enrolled
in the highest reimbursement tier — Tier 3. If you were
not covered in a group dental program within 60 days of
enrolling in a Retiree Dental Plan — or were enrolled in
a group dental program for less than 12 months — you
will be enrolled in Tier 1. After one year of coverage in
Tier 1, you will move to Tier 2. After another year, you
will be moved to Tier 3. Once enrolled in Tier 3, you
will remain in that tier for as long as you continue to be
enrolled.
The types of services covered are based on the dental
tier in which you are currently enrolled:
• Tier 1 - Diagnostic and Preventive Services Only
• Tier 2 - Includes Tier 1 Services Plus Restorative
Services
• Tier 3 - Includes Full Retiree DPO Plan Design
Retiree Dental Plans — Member Guidebook January 2024 Page 8
State Health Benets Program School Employees’ Health Benets Program
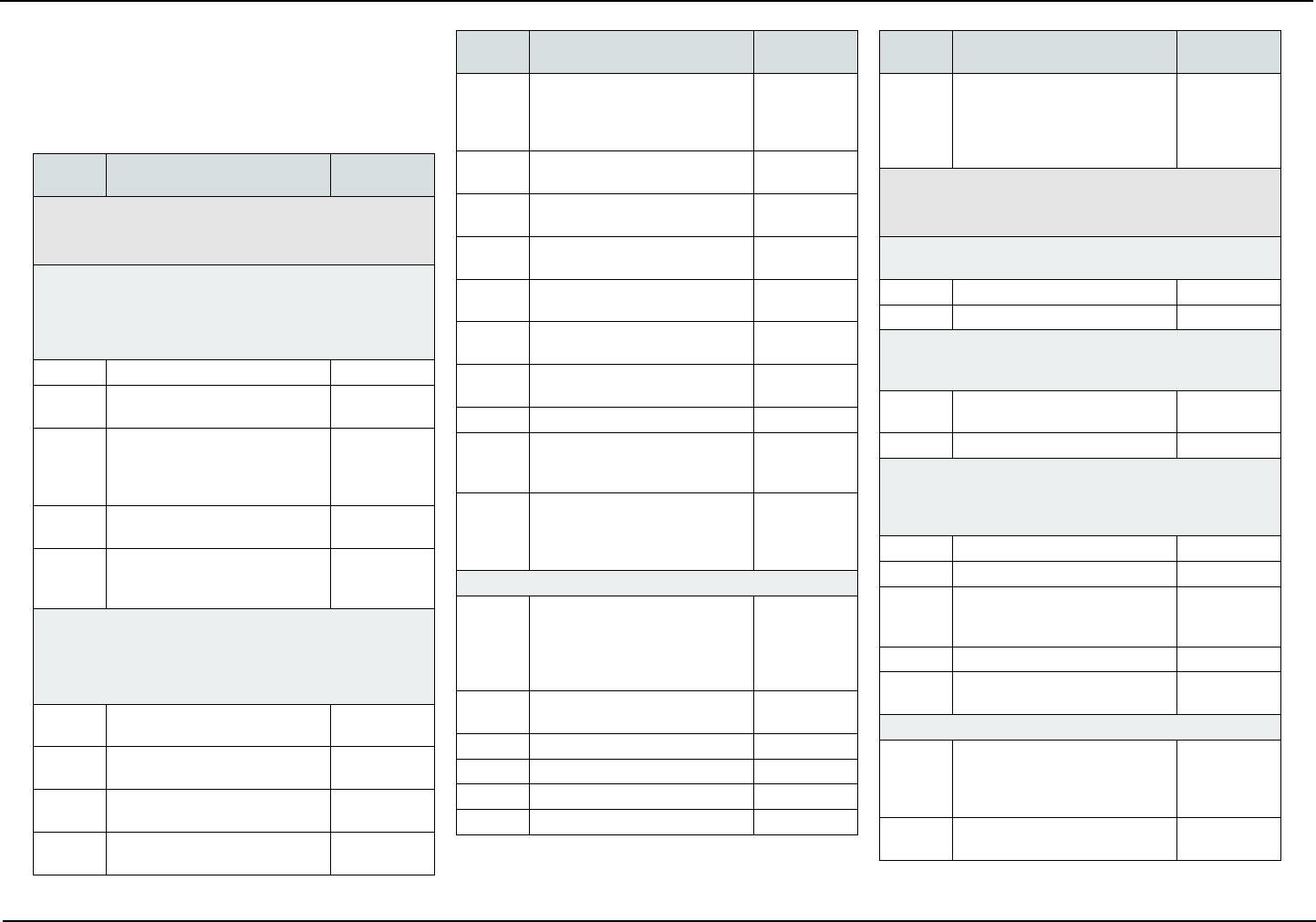
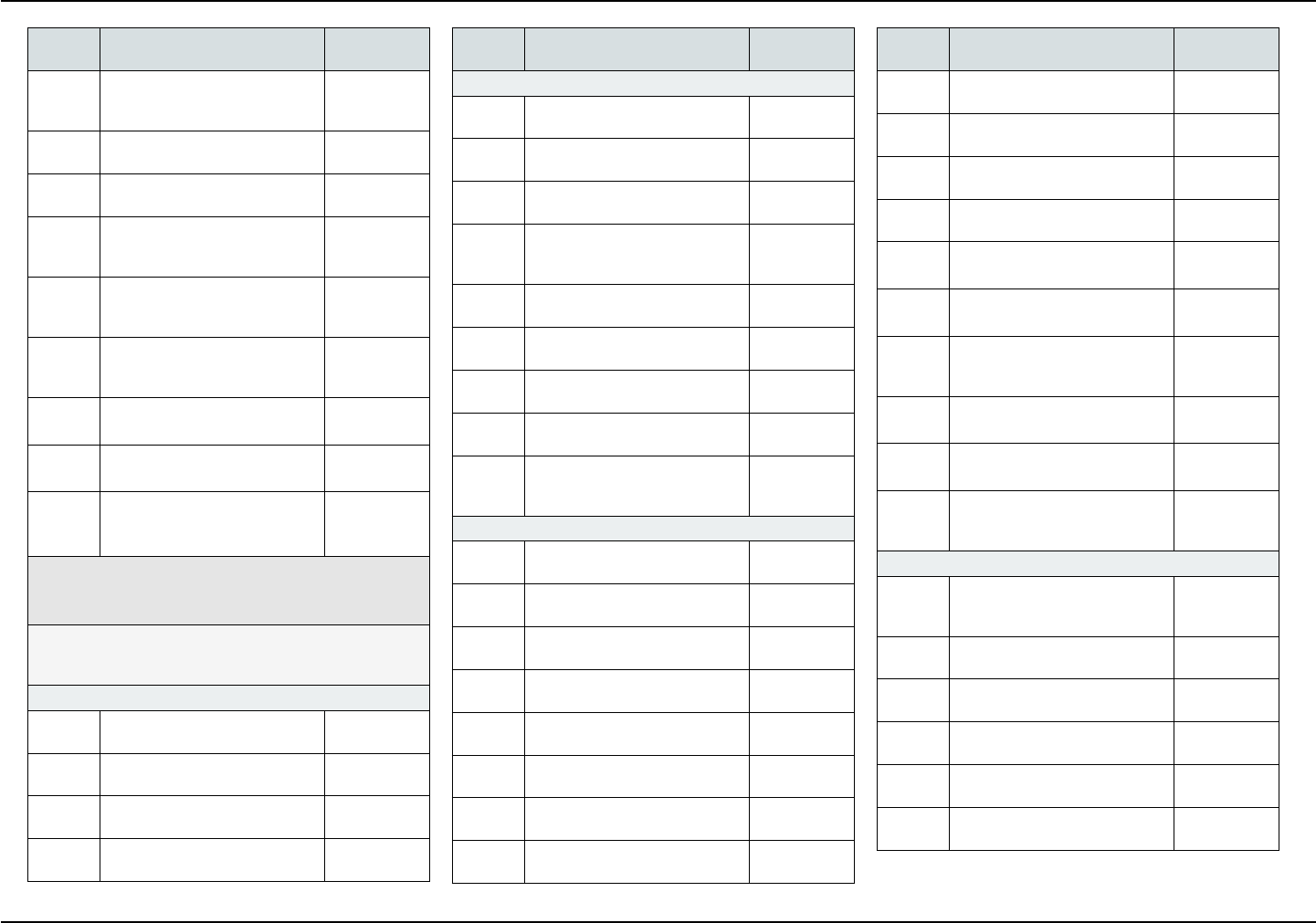
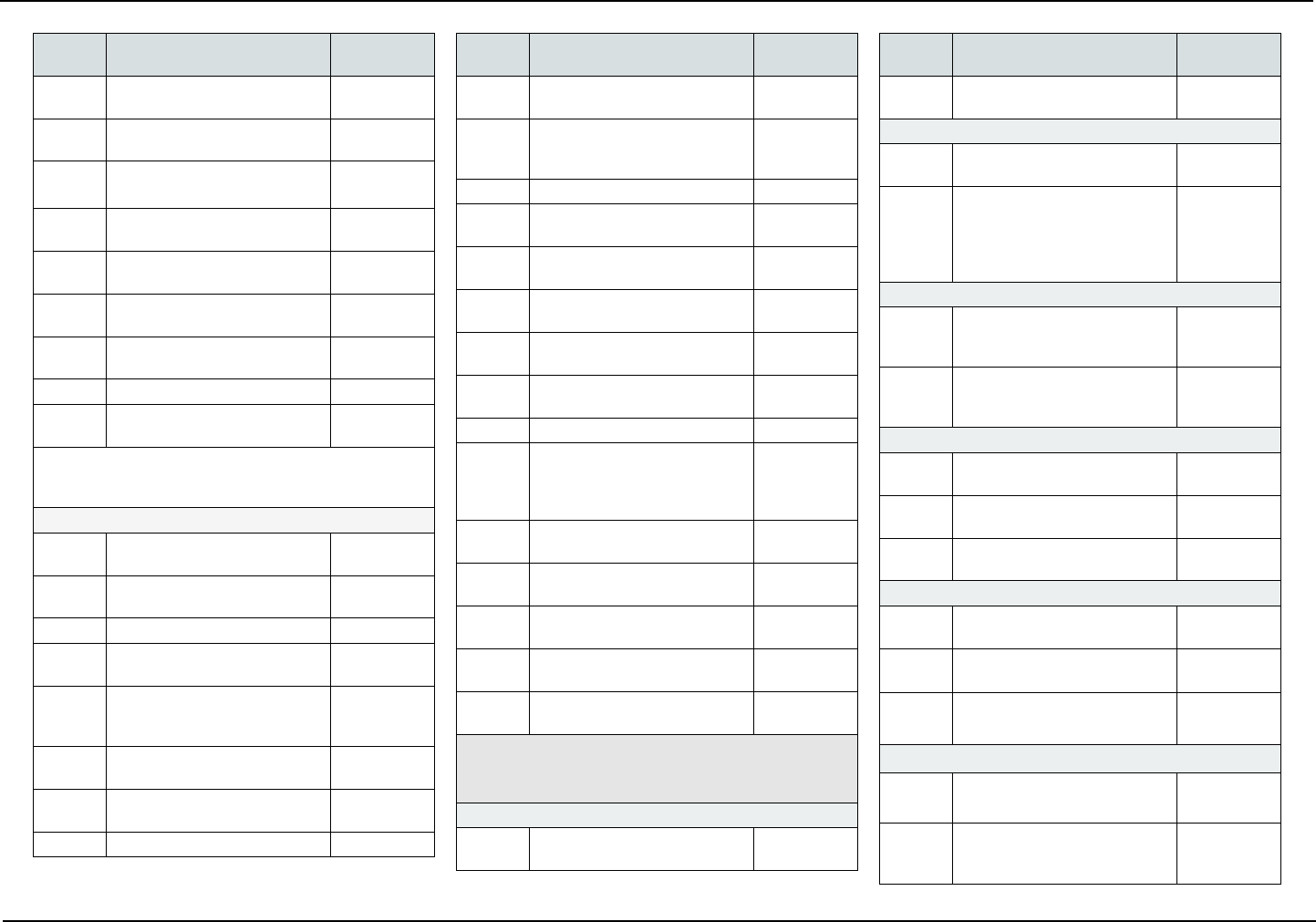
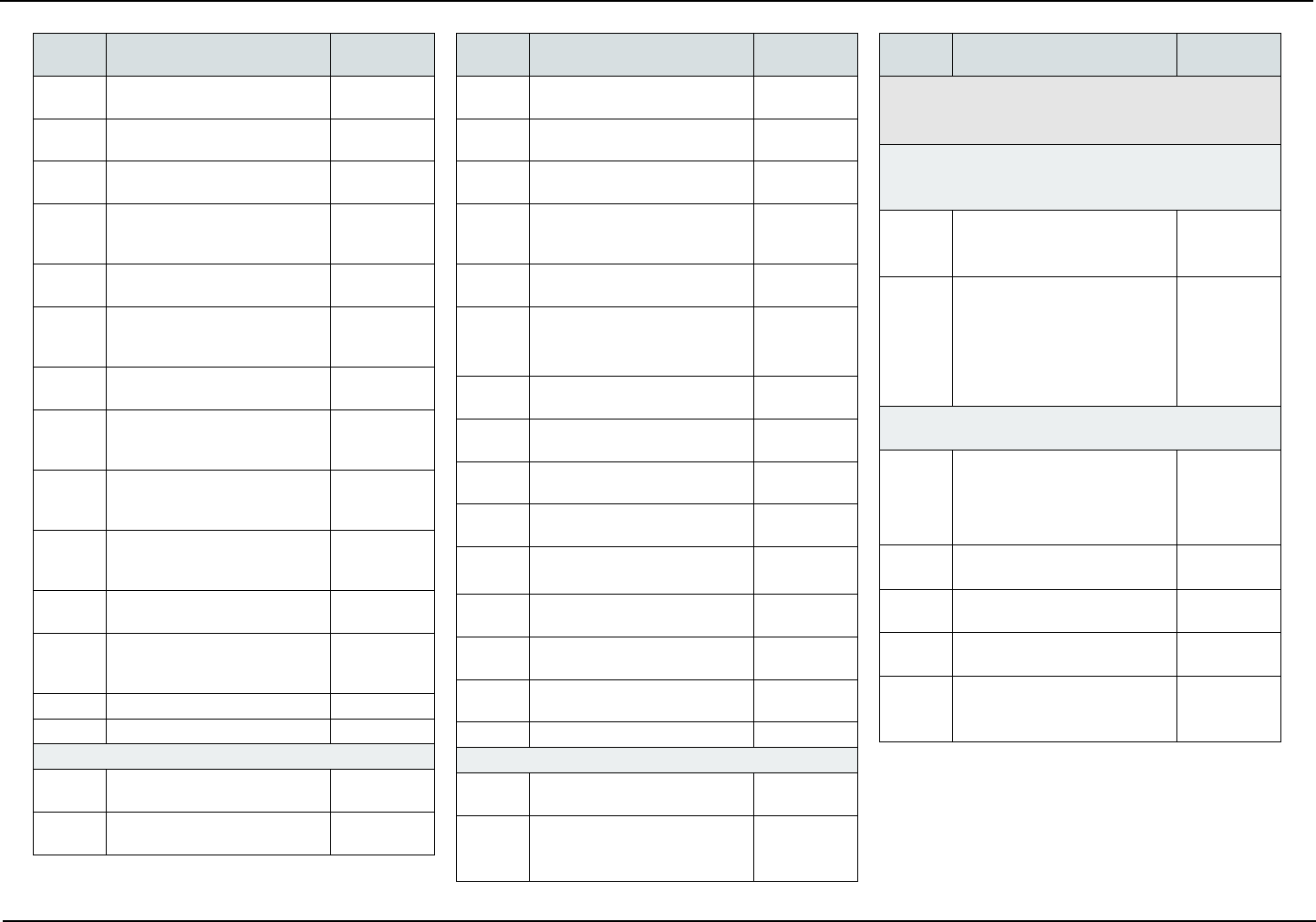
COVERED SERVICES
The following is a list of covered services and, if ap-
plicable, required copayments. Copayments are your
portion of the cost for the service.
Codes
Description of
Covered Services Copayments
D0100-D0999 I. Diagnostic
The following are covered services under Dental Tiers
1, 2, and 3.
Clinical Oral Evaluations
Oral evaluations are limited to two in a calendar year.
Emergency or limited oral evaluations are covered, limited
to one evaluation per patient, per dentist, per calendar
year. There are no copayments for diagnostic services.
D0120 Periodic Oral Evaluation $0
D0140 Limited Oral Evaluation —
Problem Focused
$0
D0145 Oral Evaluation for Patient
Under Three Years of Age
and Counseling With Primary
Caregiver
$0
D0150 Comprehensive Oral Evaluation
— New or Established Patient
$0
D0160 Detailed and Extensive Oral
Evaluation — Problem Focused,
by Report
$0
Radiographs
Bitewing X-rays are limited to two series of up to four lms
in a calendar year; set of full mouth X-rays are limited to
once per 36 month interval; no more than 18 lms per set
of mouth X-rays.
D0210 Intraoral — Complete Series of
Radiographic Images
$0
D0220 Intraoral — Periapical — First
Radiographic Image
$0
D0230 Intraoral — Periapical — Each
Additional Radiographic Image
$0
D0240 Intraoral — Occlusal Radio-
graphic Image
$0
Codes
Description of
Covered Services Copayments
D0250 Extraoral — 2D Projection Ra-
diographic Image created using
a Stationary Radiation Source
and Detector
$0
D0251 Extraoral — Posterior Dental
Radiographic Image
$0
D0270 Bitewings — Single Radio-
graphic Image
$0
D0272 Bitewings — Two Radiographic
Images
$0
D0273 Bitewings — Three Radio-
graphic Images
$0
D0274 Bitewings — Four Radiographic
Images
$0
D0277 Vertical Bitewings — Seven to
Eight Radiographic Images
$0
D0330 Panoramic Radiographic Image $0
D0340 2D Cephalometric Radio-
graphic Image — Acquisition,
Measurement and Analysis
$0
D0391 Interpretation of Diagnostic
Image by a Practitioner Not
Associated With the Capture of
the Image, Including Report
$0
Test and Laboratory Examinations
D0414 Laboratory Processing of
Microbial Specimen to Include
Culture and Sensitivity Studies,
and Preparation and Transmis-
sion of Written Report
$0
D0415 Collection of Microorganisms
for Culture and Sensitivity
$0
D0416 Viral Culture $0
D0425 Caries Susceptibility Tests $0
D0460 Pulp Vitality Tests $0
D0470 Diagnostic Casts $0
Codes
Description of
Covered Services Copayments
D0600 Non-ionizing Diagnostic Pro-
cedure Capable of Quantifying,
Monitoring, and Recording
Changes in Structure of Enam-
el, Dentin, and Cementum
$0
D1000-D1999 II. Preventive
The following are covered services under Dental Tiers
1, 2, and 3.
Dental Prophylaxis
Limited to two in a calendar year
D1110 Prophylaxis — Adult $0
D1120 Prophylaxis — Child $0
Topical Fluoride Treatment (Oce Procedure)
Limited to two in a calendar year, and only for eligible
dependent children under the age of 19 years.
D1206 Topical Application of Fluoride
Varnish
$0
D1208 Topical Application of Fluoride $0
Other Preventative Services
Sealants are limited to once per lifetime for permanent
molars of eligible dependent children under the age of 19
years.
D1330 Oral Hygiene Instruction $0
D1351 Sealant — Per Tooth $0
D1352 Preventive Resin Restoration in
a Moderate to High Caries Risk
Patient - Permanent Tooth
$0
D1353 Sealant Repair — Per Tooth $0
D1354 Interim Caries Arresting
Medicament Application
$0
Space Maintenance (Passive Appliances)
D1510 Space Maintainer — Fixed —
Unilateral Excludes a Distal
Shoe Space Maintainer - Per
Quadrant
$0
D1515 Space Maintainer — Fixed —
Bilateral
$0
Page 9 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
Codes
Description of
Covered Services Copayments
D1520 Space Maintainer —
Removable — Unilateral - Per
Quadrant
$0
D1525 Space Maintainer —
Removable — Bilateral
$0
D1551 Re-Cement or Re-Bond Bilater-
al Space Maintainer - Maxillary
$0
D1552 Re-Cement or Re-Bond
Bilateral Space Maintainer -
Mandibular
$0
D1553 Re-Cement or Re-Bond Bilat-
eral Space Maintainer - Per
Quadrant
$0
D1556 Removal of Fixed Unilateral
Space Maintainer - Per Quad-
rant
$0
D1557 Removal of Fixed Unilateral
Space Maintainer - Maxillary
$0
D1558 Removal of Fixed Unilateral
Space Maintainer - Mandibular
$0
D1575 Distal Shoe Space Maintain-
er — Fixed — Unilateral - Per
Quadrant
$0
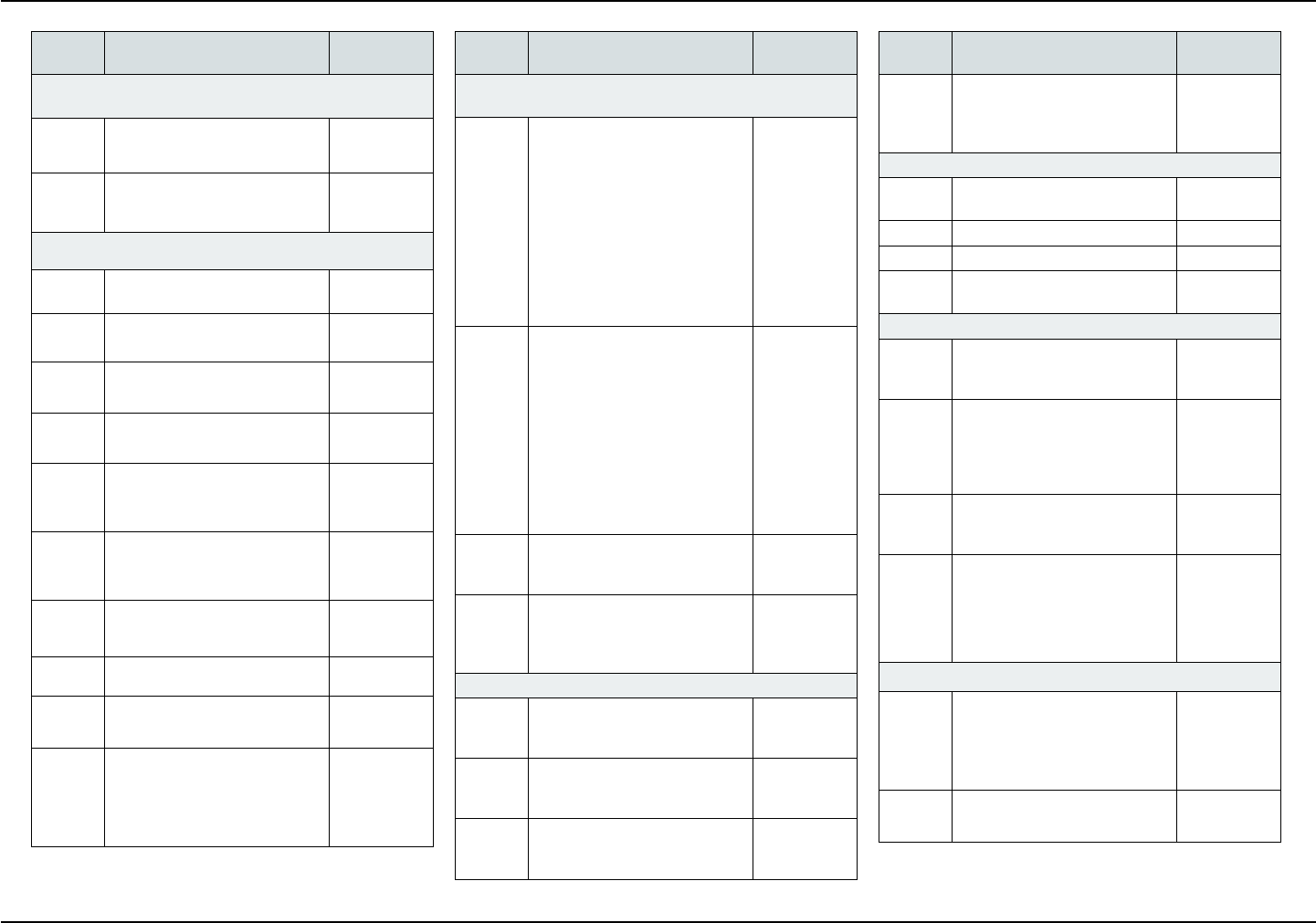
D2000-D2999 III. Restorative
The following are covered services under Dental Tiers
2 and 3 only.
The replacement of a crown is covered only after a ve-year
period measured from the date on which the crown was pre-
viously placed.
Amalgam Restorations (Including Polishing)
D2140 Amalgam — One Surface —
Primary or Permanent
$15
D2150 Amalgam — Two Surfaces —
Primary or Permanent
$20
D2160 Amalgam — Three Surfaces —
Primary or Permanent
$25
D2161 Amalgam — Four or More Sur-
faces — Primary or Permanent
$30
Codes
Description of
Covered Services Copayments
Resin Restorations
D2330 Resin-Based Composite —
One Surface — Anterior
$25
D2331 Resin-Based Composite —
Two Surfaces — Anterior
$30
D2332 Resin-Based Composite —
Three Surfaces — Anterior
$35
D2335 Resin-Based Composite —
Four or More Surfaces or In-
volving Incisal Angle — Anterior
$45
D2390 Resin-Based Composite Crown
— Anterior
$55
D2391 Resin-Based Composite —
One Surface — Posterior
$25
D2392 Resin-Based Composite —
Two Surfaces — Posterior
$40
D2393 Resin-Based Composite —
Three Surfaces — Posterior
$55
D2394 Resin-Based Composite
— Four or More Surfaces —
Posterior
$70
Inlay/Onlay Restorations
D2510 Inlay — Metallic —
One Surface
$150
D2520 Inlay — Metallic —
Two Surfaces
$150
D2530 Inlay — Metallic —
Three or More Surfaces
$150
D2542 Onlay — Metallic —
Two Surfaces
$150
D2543 Onlay — Metallic — Three
Surfaces
$150
D2544 Onlay — Metallic — Four or
More Surfaces
$150
D2610 Inlay — Porcelain/Ceramic —
One Surface
$175
D2620 Inlay — Porcelain/Ceramic —
Two Surfaces
$175
Codes
Description of
Covered Services Copayments
D2630 Inlay — Porcelain/Ceramic —
Three or More Surfaces
$175
D2642 Onlay — Porcelain/Ceramic —
Two Surfaces
$175
D2643 Onlay — Porcelain/Ceramic —
Three Surfaces
$175
D2644 Onlay — Porcelain/Ceramic —
Four or More Surfaces
$175
D2650 Inlay — Resin-Based
Composite — One Surface
$160
D2651 Inlay — Resin-Based
Composite — Two Surfaces
$160
D2652 Inlay — Resin-Based
Composite — Three or More
Surfaces
$160
D2662 Onlay — Resin-Based Com-
posite — Two Surfaces
$160
D2663 Onlay — Resin-Based
Composite — Three Surfaces
$160
D2664 Onlay — Resin-Based
Composite — Four or More
Surfaces
$160
Crowns — Single Restorations Only
D2710 Crown — Resin-Based
Composite (Indirect)
See Note
$175
D2720 Crown — Resin With High
Noble Metal
$235
D2721 Crown — Resin With
Predominantly Base Metal
$225
D2722 Crown — Resin With Noble
Metal
$225
D2740 Crown — Porcelain/Ceramic
Substrate
$295
D2750 Crown — Porcelain Fused to
High Noble Metal
$340
Retiree Dental Plans — Member Guidebook January 2024 Page 10
State Health Benets Program School Employees’ Health Benets Program
Codes
Description of
Covered Services Copayments
D2751 Crown — Porcelain Fused to
Predominantly Base Metal
$295
D2752 Crown — Porcelain Fused to
Noble Metal
$295
D2753 Crown - Porcelain Fused to
Titanium and Titanium Alloys
$295
D2780 Crown — 3/4 Cast High Noble
Metal
$340
D2781 Crown — 3/4 Cast
Predominantly Base Metal
$295
D2790 Crown — Full Cast High Noble
Metal
$340
D2791 Crown — Full Cast
Predominantly Base Metal
$295
D2792 Crown — Full Cast Noble Metal $295
D2794 Crown — Titanium and Titani-
um Alloys
$340
Note: There is no copayment for procedure D2710 when
performed in conjunction with a permanent crown on the
same tooth.
Other Restorative Services
D2910 Recement Inlay, Onlay, or
Partial Coverage Restoration
$15
D2915 Recement Cast or
Prefabricated Post and Core
$15
D2920 Recement Crown $15
D2921 Reattachment of Tooth
Fragment Incisal Edge or Cusp
$0
D2929 Prefabricated Porcelain/
Ceramic Crown —
Primary Tooth
$69
D2930 Prefabricated Stainless Steel
Crown — Primary Tooth
$55
D2931 Prefabricated Stainless Steel
Crown — Permanent Tooth
$55
D2932 Prefabricated Resin Crown $55
Codes
Description of
Covered Services Copayments
D2933 Prefabricated Stainless Steel
Crown With Resin Window
$55
D2934 Prefabricated Esthetic Coated
Stainless Steel Crown —
Primary Tooth
$55
D2940 Protective Restoration $20
D2941 Interim Therapeutic Restoration
— Primary Dentition
$0
D2950 Core Buildup, Including any
Pins
$45
D2951 Pin Retention — Per Tooth in
Addition to Restoration
$15
D2952 Cast Post and Core in Addition
to Crown
$60
D2954 Prefabricated Post and Core in
Addition to Crown
$60
D2955 Post Removal $45
D2971 Additional Procedures to
Construct New Crown under
Existing Partial Denture
Framework
$20
D2980 Crown Repair Necessitated by
Restorative Material Failure
$15
D2981 Inlay Repair Necessitated by
Restorative Material Failure
$15
D2982 Onlay Repair Necessitated by
Restorative Material Failure
$15
D2983 Veneer Repair Necessitated by
Restorative Material Failure
$15
D2990 Resin Inltration of Incipient
Smooth Surface Lesions
$15
D3000-D3999 IV. Endodontics
The following are covered services under Dental Tier
3 only.
Pulp Capping
D3110 Pulp Capping — Direct —
Excluding Final Restoration
$15
Codes
Description of
Covered Services Copayments
D3120 Pulp Capping — Indirect —
Excluding Final Restoration
$15
Pulpotomy
D3220 Therapeutic Pulpotomy —
Excluding Final Restoration
$35
D3222 Therapeutic Pulpotomy —
Partial Pulpotomy for
Apexogenesis — Permanent
Tooth With Incomplete Root
Development
$35
Endodontic Therapy on Primary Teeth
D3230 Pulpal Therapy (Resorbable Fill-
ing) — Anterior-Primary Tooth —
Excluding Final Restoration
$35
D3240 Pulpal Therapy (Resorbable Fill-
ing) — Posterior-Primary Tooth —
Excluding Final Restoration
$35
Endodontic Therapy
D3310 Anterior (Excluding Final
Restoration)
$150
D3320 Bicuspid (Excluding Final
Restoration)
$190
D3330 Molar (Excluding Final Resto-
ration)
$225
Endodontic Retreatment
D3346 Retreatment of Previous Root
Canal Therapy — Anterior
$190
D3347 Retreatment of Previous Root
Canal Therapy — Bicuspid
$225
D3348 Retreatment of Previous Root
Canal Therapy — Molar
$265
Apexication/Recalcication Procedures
D3351 Apexication/Recalcication —
Initial Visit
$55
D3352 Apexication/Recalcication —
Interim Medication
Replacement
$55
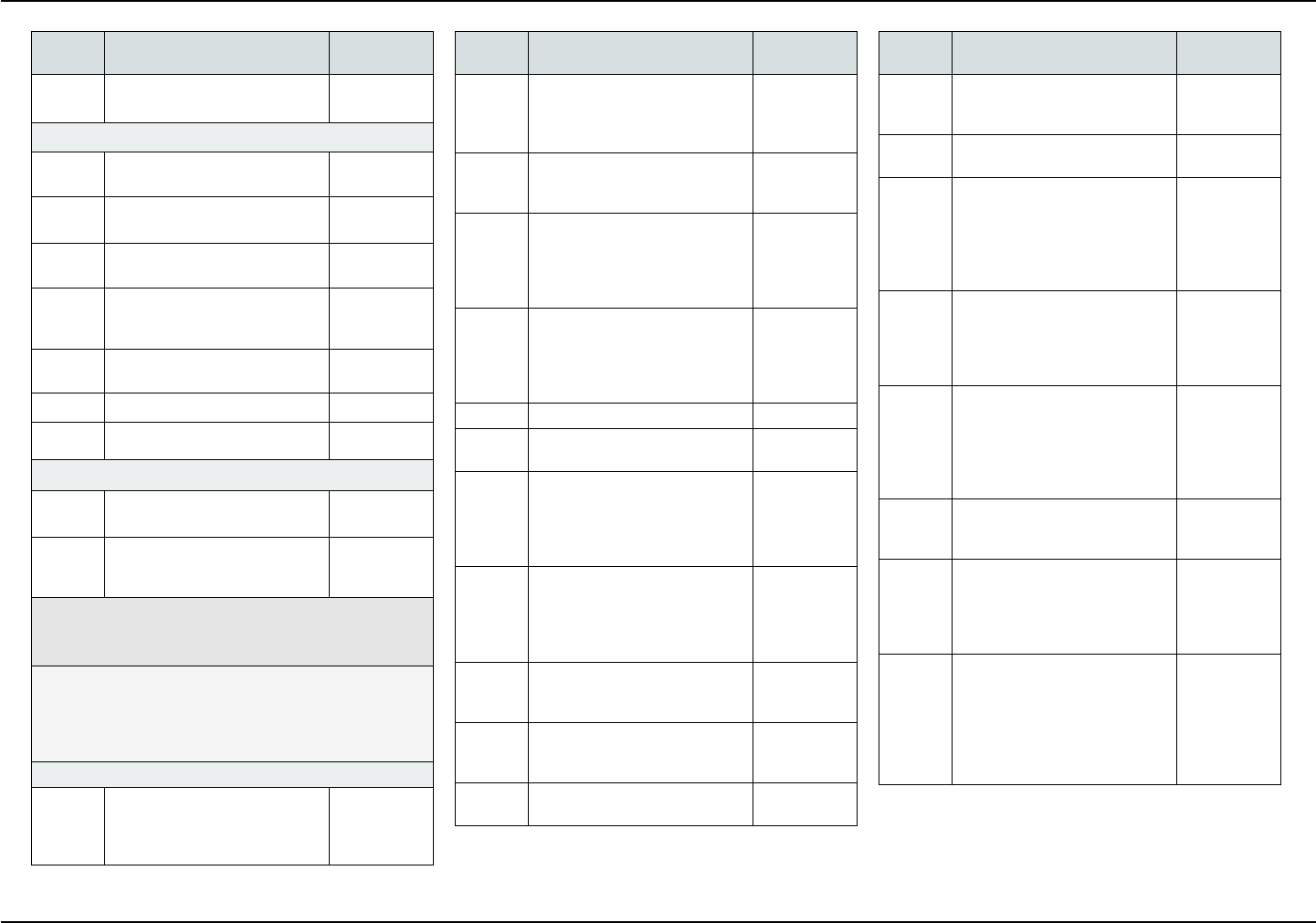
Page 11 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
Codes
Description of
Covered Services Copayments
D3353 Apexication/Recalcication —
Final Visit
$55
Apicoectomy/Periapical Services
D3410 Apicoectomy/Periradicular
Surgical — Anterior
$135
D3421 Apicoectomy/Periradicular
Surgical — Bicuspid First Root
$135
D3425 Apicoectomy/Periradicular
Surgical — Molar First Root
$135
D3426 Apicoectomy/Periradicular
Surgical — Each Additional
Root
$60
D3427 Periradicular Surgical —
Without Apicoectomy
$135
D3430 Retrograde Filling — Per Root $35
D3450 Root Amputation — Per Root $60
Other Endodontic Procedures
D3910 Surgical Procedure for Isolation
of Tooth With Rubber Dam
$15
D3920 Hemisection (Including any
Root Removal) — Not Including
Root Canal Therapy
$80
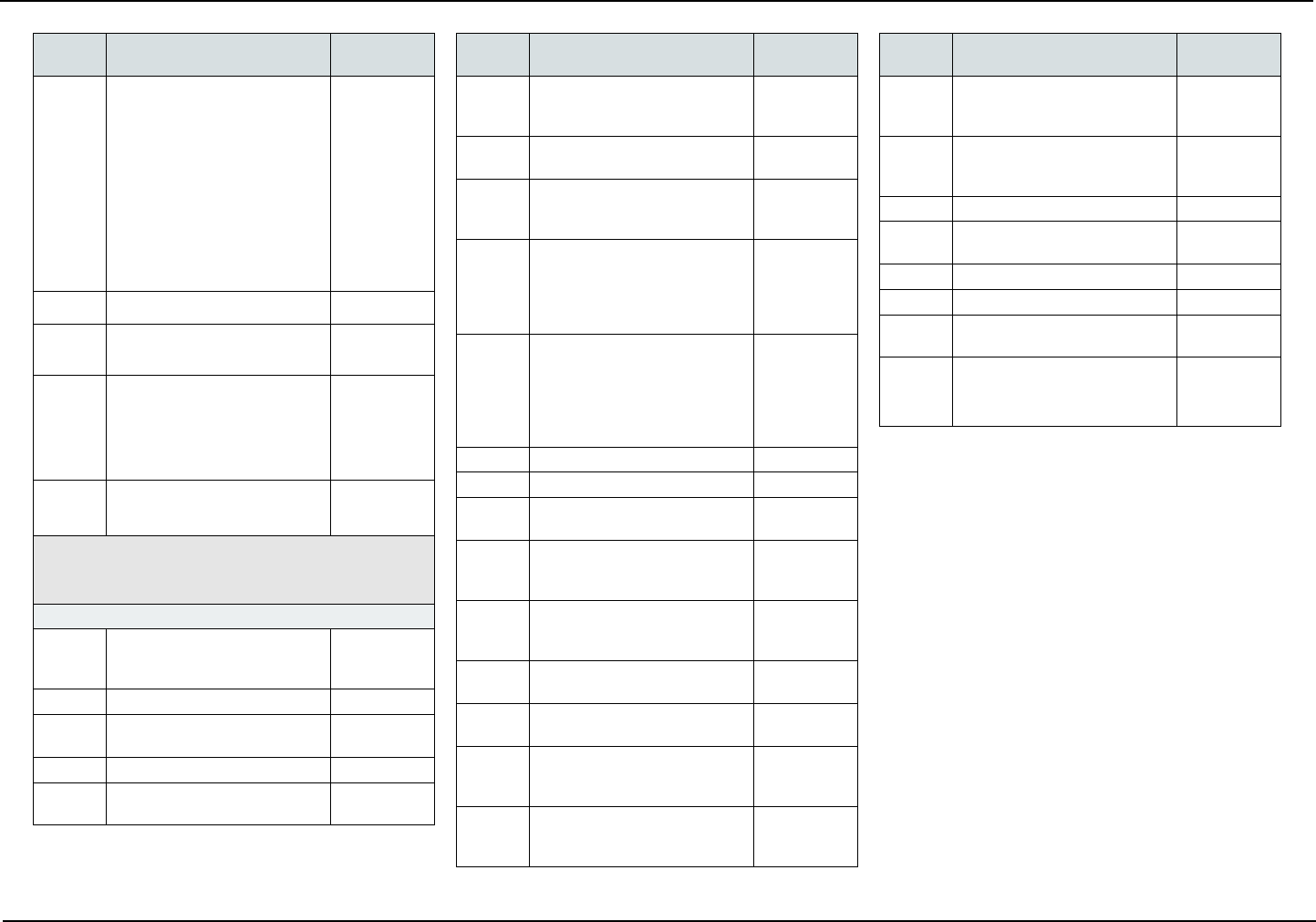
D4000-D4999 V. Periodontics
The following are covered services under Dental Tier
3 only.
Coverage for surgical periodontal procedures, excluding
scaling and root planing, is limited to one surgical periodontal
treatment per quadrant every 36 months; coverage for scal-
ing and root planing is limited to one nonsurgical periodontal
treatment per quadrant every 12 months.
Surgical Services
D4210 Gingivectomy or
Gingivoplasty — Four or more
Contiguous Teeth or Tooth
Bounded Spaces per Quadrant
$135
Codes
Description of
Covered Services Copayments
D4211 Gingivectomy or Gingivoplasty
— One to Three Contiguous
Teeth or Tooth Bounded
Spaces per Quadrant
$90
D4212 Gingivectomy or Gingivoplasty
to Allow Access for Restorative
Procedure — Per Tooth
$12
D4240 Gingival Flap Procedure
Including Root Planing — Four
or more Contiguous Teeth or
Tooth Bounded Spaces per
Quadrant
$160
D4241 Gingival Flap Procedure
including Root Planing — One
to Three Contiguous Teeth or
Tooth Bounded Spaces per
Quadrant
$90
D4245 Apically Positioned Flap $130
D4249 Clinical Crown Lengthening —
Hard Tissue
$160
D4260 Osseous Surgery (Including
Flap Entry and Closure) — Four
or more Contiguous Teeth or
Tooth Bounded Spaces per
Quadrant
$265
D4261 Osseous Surgery (Including
Flap Entry and Closure) — One
to Three Contiguous Teeth or
Tooth Bounded Spaces per
Quadrant
$150
D4263 Bone Replacement Graft —
Retained Natural Tooth — First
Site in Quadrant
$135
D4264 Bone Replacement Graft —
Retained Natural Tooth — Each
Additional Site in Quadrant
$75
D4266 Guided Tissue Regeneration —
Resorbable Barrier per Site
$120
Codes
Description of
Covered Services Copayments
D4267 Guided Tissue Regeneration —
Non-resorbable Barrier per Site
(Includes Membrane Removal)
$135
D4270 Pedicle Soft Tissue Graft
Procedure
$235
D4273 Autogenous Connective Tissue
Graft Procedures (Including
Donor and Recipient Surgical
Sites) — First Tooth, Implant,
or Edentulous Tooth Position
in Graft
$250
D4274 Mesial/Distal Procedure —
Single Tooth (When not Per-
formed in Conjunction With
Surgical Procedures in the
same Anatomical Area)
$100
D4275 Non-Autogenous Connective
Tissue Graft (Including
Recipient Site and Donor Ma-
terial) — First Tooth, Implant,
or Edentulous Tooth Position
in Graft
$235
D4276 Combined Connective Tissue
and Double Pedicle Graft —
Per Tooth
$235
D4277 Free Soft Tissue Graft Proce-
dure (Including Recipient and
Donor Surgical Sites) — First
Tooth, Implant, or Edentulous
Tooth Position in a Graft
$70
D4278 Free Soft Tissue Graft
Procedure (Including Recipient
and Donor Surgical Sites) —
Each additional Contiguous
Tooth, Implant, or Edentulous
Tooth Position in same Graft
Site
$35
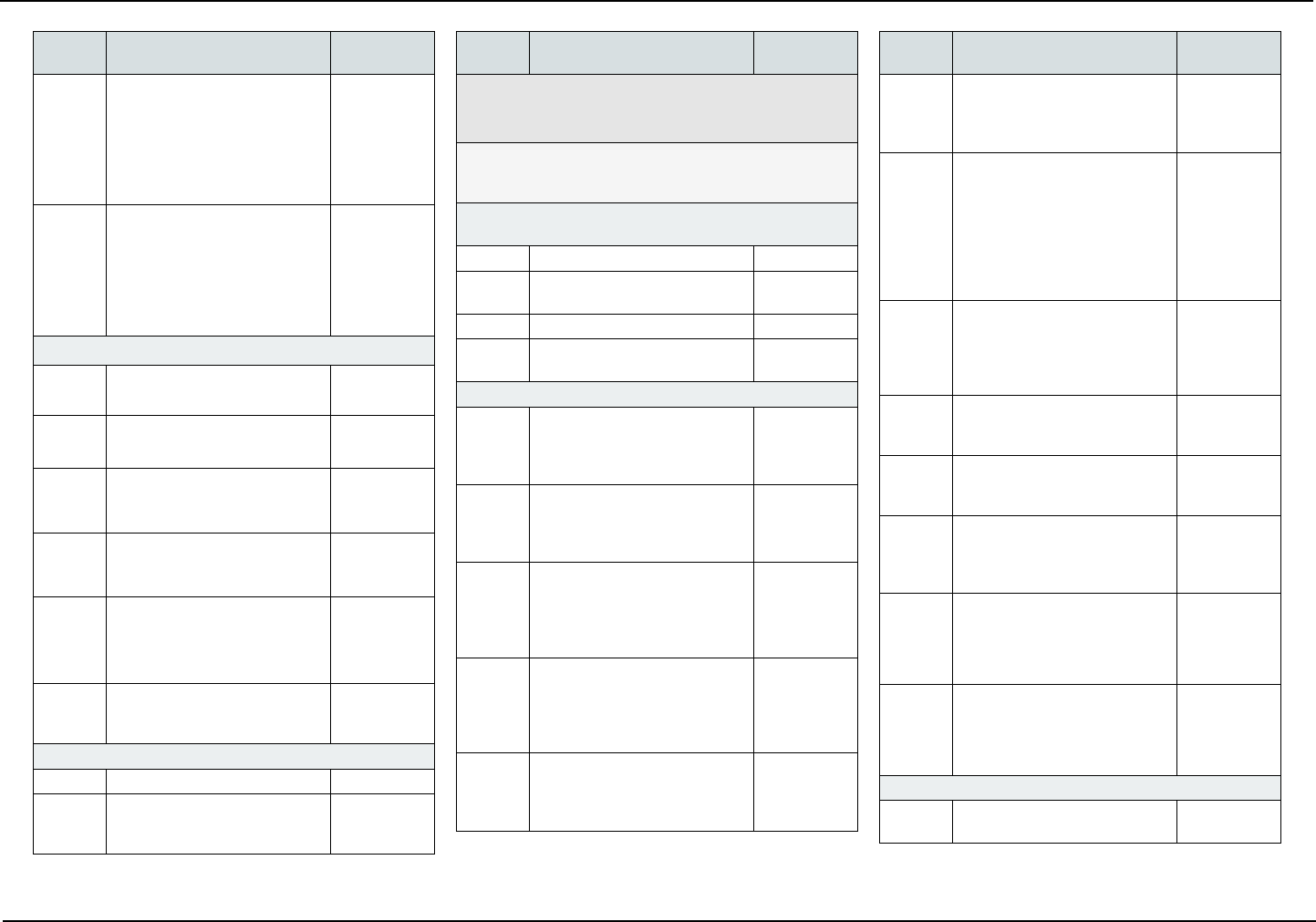
Retiree Dental Plans — Member Guidebook January 2024 Page 12
State Health Benets Program School Employees’ Health Benets Program
Codes
Description of
Covered Services Copayments
D4283 Autogenous Connective Tissue
Graft Procedure (Including
Donor and Recipient Surgi-
cal Sites) — Each additional
Contiguous Tooth, Implant, or
Edentulous Tooth Position in
same Graft Site
$138
D4285 Non-Autogenous Connective
Tissue Graft Procedure (In-
cluding Recipient Surgical Site
and Donor Material) — Each
Additional Contiguous Tooth,
Implant, or Edentulous Tooth
Position in same Graft Site
$129
Non-Surgical Periodontal Services
D4320 Provisional Splinting —
Intracoronal
$25
D4321 Provisional Splinting —
Extracoronal
$25
D4341 Periodontal Scaling and Root
Planing — Four or More Teeth
per Quadrant
$70
D4342 Periodontal Scaling or Root
Planing — One to Three Teeth
per Quadrant
$40
D4346 Scaling in Presence of Gen-
eralized Moderate or Severe
Gingival Inammation — Full
Mouth, after Oral Evaluation
$20
D4355 Full Mouth Debridement to En-
able Comprehensive Periodon-
tal Evaluation and Diagnosis
$40
Other Periodontal Services
D4910 Periodontal Maintenance $40
D4920 Unscheduled Dressing Change
(By someone other than Treat-
ing Dentist)
$15
Codes
Description of
Covered Services Copayments
D5000-D5899 VI. Prosthodontics (Removable)
The following are covered services under Dental Tier
3 only.
The replacement of an existing removable prosthetic appli-
ance is covered only after a ve-year period measured from
the date on which the appliance was previously placed.
Complete Dentures
Including Routine Post Delivery Care
D5110 Complete Denture — Maxillary $340
D5120 Complete Denture —
Mandibular
$340
D5130 Immediate Denture — Maxillary $370
D5140 Immediate Denture —
Mandibular
$370
Partial Dentures Including Routine Post Delivery Care
D5211 Maxillary Partial Denture —
Resin Base (Including any
Conventional Clasps, Rests,
and Teeth)
$370
D5212 Mandibular Partial Denture
— Resin Base (Including any
Conventional Clasps, Rests,
and Teeth)
$370
D5213 Maxillary Partial Denture —
Cast Metal Framework w/
Resin Denture Bases (Including
Retentive/Clasping Materials,
Rests, and Teeth)
$405
D5214 Mandibular Partial Denture —
Cast Metal Framework With
Resin Denture Bases (Including
Retentive/Clasping Materials,
Rests, and Teeth)
$405
D5221 Immediate Maxillary Partial
Denture — Resin Base
(Including Retentive/Clasping
Materials, Rests, and Teeth)
$426
Codes
Description of
Covered Services Copayments
D5222 Immediate Mandibular Partial
Denture — Resin Base
(Including Retentive/Clasping
Materials, Rests, and Teeth)
$426
D5223 Immediate Maxillary Partial
Denture — Cast Metal
Framework With Resin Denture
Bases (Including Retentive/
Clasping Materials, Rests,
and Teeth) Includes limited
Follow-up Care Only; Does not
Include Future Rebasing
$466
D5224 Immediate Mandibular Partial
Denture — Cast Metal Frame-
work With Resin Denture Bases
(Including Retentive/Clasping
Materials, Rests, and Teeth)
$466
D5225 Maxillary Partial Denture —
Flexible Base (Including any
Clasps, Rests, and Teeth)
$445
D5226 Mandibular Partial Denture —
Flexible Base (Including any
Clasps, Rests, and Teeth)
$445
D5281 Removable Unilateral Partial
Denture — One Piece Cast
Metal (Including Clasps and
Teeth)
$205
D5284 Removable Unilateral Partial
Denture - One Piece Flexible
Base (Including Clasps and
teeth) - Per Quadrant
$223
D5286 Removable Unilateral Partial
Denture - One Piece Resin
(Including Clasps and teeth) -
Per Quadrant
$185
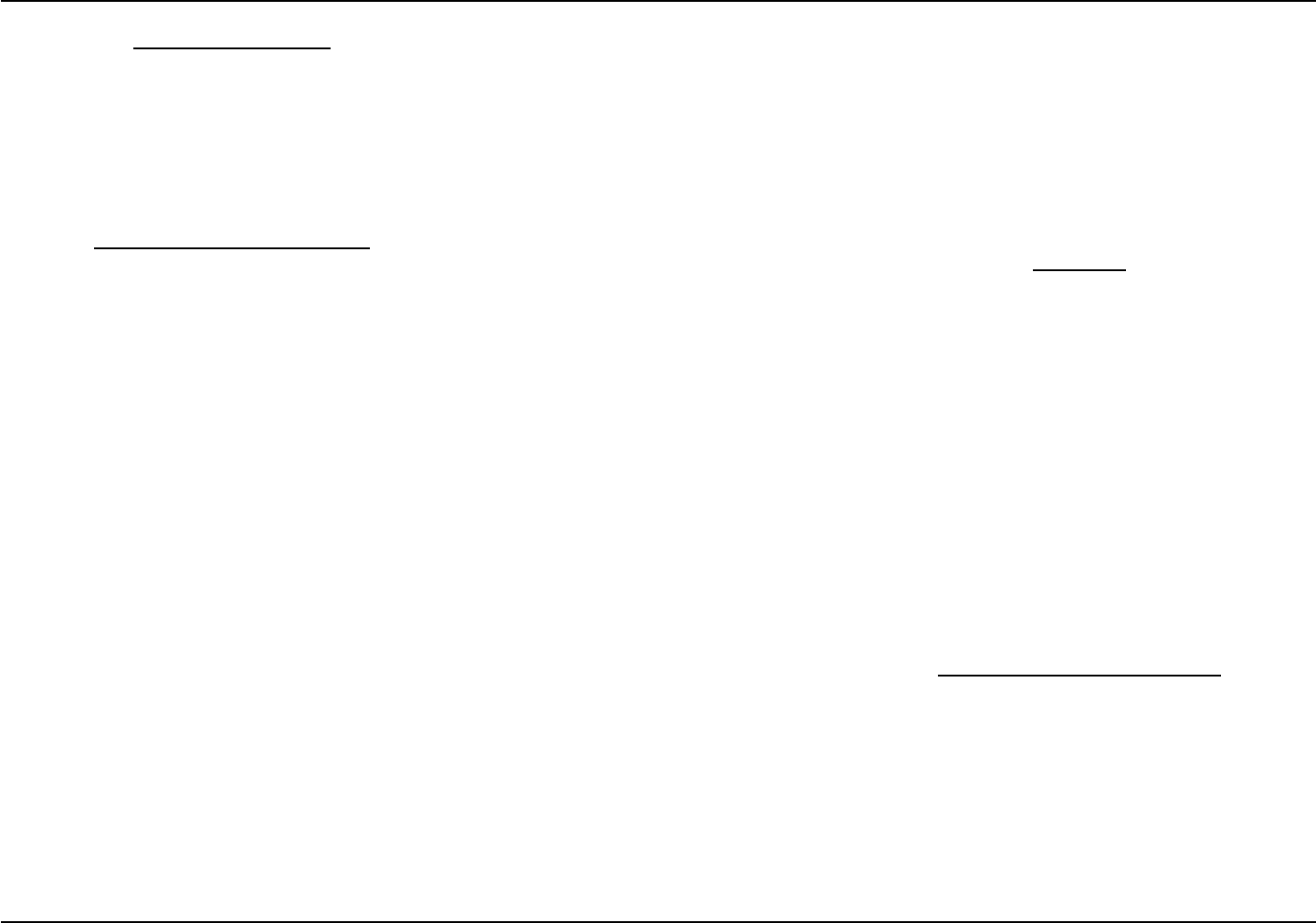
Adjustments to Removable Prostheses
D5410 Adjust Complete Denture —
Maxillary
$15
Page 13 January 2024 Retiree Dental Plans — Member Guidebook
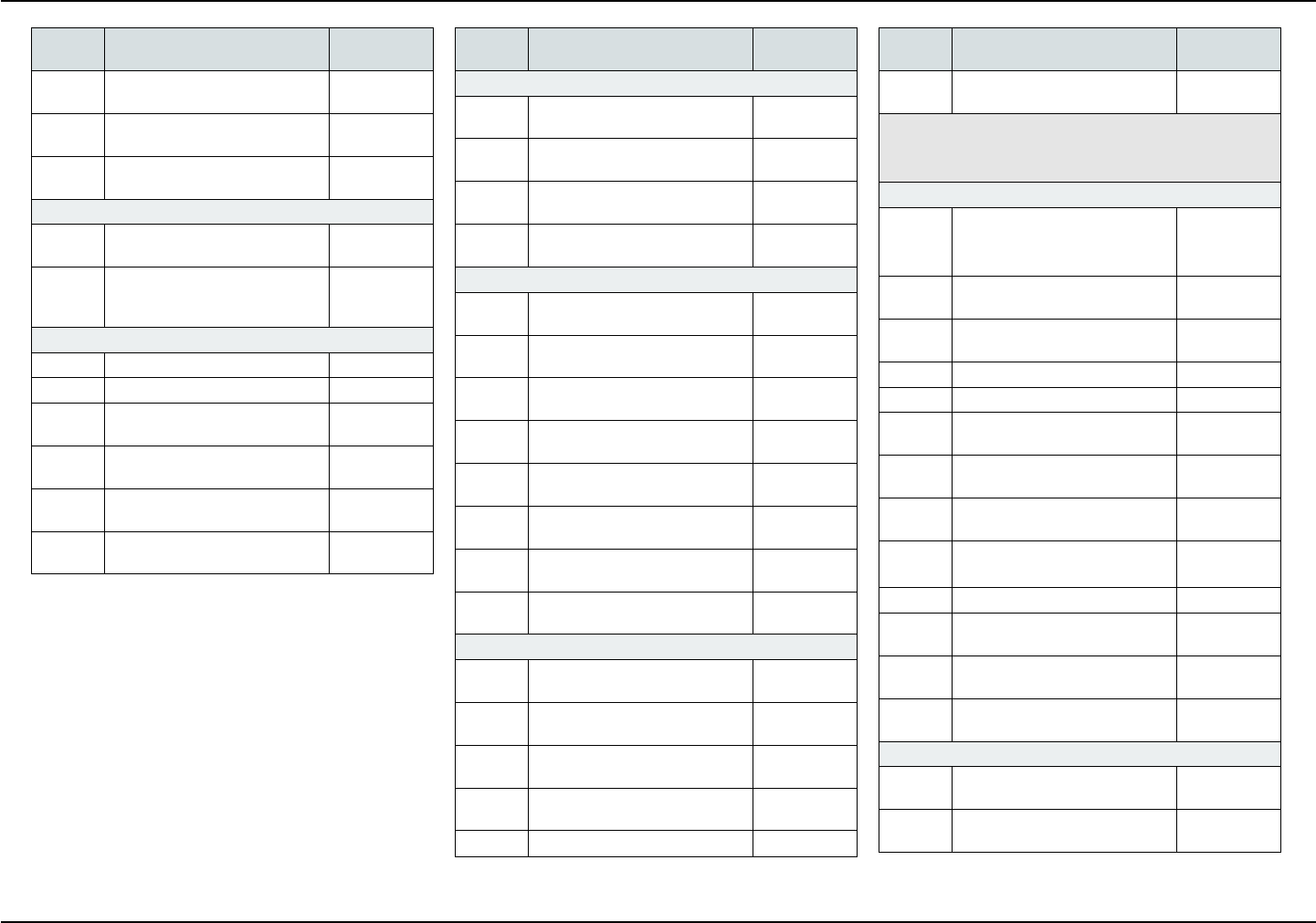
School Employees’ Health Benets Program State Health Benets Program
Codes
Description of
Covered Services Copayments
D5411 Adjust Complete Denture —
Mandibular
$15
D5421 Adjust Partial Denture —
Maxillary
$15
D5422 Adjust Partial Denture —
Mandibular
$15
Repairs to Complete Dentures
D5510 Repair Broken Complete
Denture Base
$55
D5520 Replace Missing or Broken
Teeth — Complete Denture —
Each Tooth
$55
Repairs to Partial Dentures
D5610 Repair Resin Denture Base $55
D5620 Repair Cast Framework $55
D5630 Repair or Replace Broken
Clasp — Per Tooth
$55
D5640 Replace Broken Teeth — Per
Tooth
$55
D5650 Add Tooth to Existing Partial
Denture
$55
D5660 Add Clasp to Existing Partial
Denture — Per Tooth
$55
Codes
Description of
Covered Services Copayments
Denture Rebase Procedures
D5710 Rebase Complete Maxillary
Denture
$130
D5711 Rebase Complete Mandibular
Denture
$130
D5720 Rebase Maxillary Partial
Denture
$130
D5721 Rebase Mandibular Partial
Denture
$130
Denture Reline Procedures
D5730 Reline Complete Maxillary
Denture — Chairside
$60
D5731 Reline Complete Mandibular
Denture — Chairside
$60
D5740 Reline Maxillary Partial Denture
— Chairside
$60
D5741 Reline Mandibular Partial Den-
ture — Chairside
$60
D5750 Reline Complete Maxillary
Denture — (Lab Process)
$60
D5751 Reline Complete Mandibular
Denture — (Lab Process)
$60
D5760 Reline Maxillary Partial Denture
— (Lab Process)
$60
D5761 Reline Mandibular Partial Den-
ture — (Lab Process)
$60
Other Removable Prosthetic Services
D5810 Interim Complete Denture
(Maxillary)
$75
D5811 Interim Complete Denture
(Mandibular)
$75
D5820 Interim Partial Denture
(Maxillary)
$60
D5821 Interim Partial Denture
(Mandibular)
$60
D5850 Tissue Conditioning (Maxillary) $55
Codes
Description of
Covered Services Copayments
D5851 Tissue Conditioning
(Mandibular)
$55
D6200-D6999 VII. Prosthodontics, Fixed
The following are covered services under Dental Tier
3 only.
Fixed Partial Denture Pontics
D6097 Abutment Supported Crown
- Porcelain Fused to Titanium
and Titanium Alloys
$295
D6210 Pontic — Cast High Noble
Metal
$340
D6211 Pontic — Cast Predominantly
Base Metal
$295
D6212 Pontic — Cast Noble Metal $295
D6214 Pontic — Titanium $340
D6240 Pontic — Porcelain Fused to
High Noble Metal
$340
D6241 Pontic — Porcelain Fused to
Predominantly Base Metal
$295
D6242 Pontic — Porcelain Fused to
Noble Metal
$295
D6243 Pontic - Porcelain Fused to
Titanium and Titanium Alloys
$295
D6245 Pontic — Porcelain/Ceramic $295
D6250 Pontic — Resin With High
Noble Metal
$225
D6251 Pontic — Resin With
Predominantly Base Metal
$225
D6252 Pontic — Resin With Noble
Metal
$225
Fixed Partial Denture Retainers — Inlays/Onlays
D6545 Retainer — Cast Metal for Res-
in Bonded Fixed Prosthesis
$150
D6549 Resin Retainer — For Resin
Bonded Fixed Prosthesis
$75
Retiree Dental Plans — Member Guidebook January 2024 Page 14
State Health Benets Program School Employees’ Health Benets Program
Codes
Description of
Covered Services Copayments
D6602 Inlay — Cast High Noble Metal
— Two Surfaces
$265
D6603 Inlay — Cast High Noble Metal
— Three or More Surfaces
$265
D6604 Inlay — Cast Predominantly
Base Metal — Two Surfaces
$160
D6605 Inlay — Cast Predominantly
Base Metal — Three or More
Surfaces
$160
D6606 Inlay — Cast Noble Metal —
Two Surfaces
$230
D6607 Retainer Inlay — Cast Noble
Metal — Three or More
Surfaces
$230
D6610 Retainer Onlay — Cast High
Noble Metal — Two Surfaces
$275
D6611 Retainer Onlay — Cast High
Noble Metal — Three or More
Surfaces
$275
D6612 Retainer Onlay — Cast Pre-
dominantly Base Metal — Two
Surfaces
$160
D6613 Retainer Onlay — Cast
Predominantly Base Metal —
Three or More Surfaces
$160
D6614 Retainer Onlay — Cast Noble
Metal — Two Surfaces
$265
D6615 Retainer Onlay — Cast Noble
Metal — Three or More
Surfaces
$265
D6624 Retainer Inlay — Titanium $265
D6634 Retainer Onlay — Titanium $275
Fixed Partial Denture Retainers — Crown
D6720 Retainer Crown — Resin With
High Noble Metal
$225
D6721 Retainer Crown — Resin With
Predominantly Base Metal
$225
Codes
Description of
Covered Services Copayments
D6722 Retainer Crown — Resin With
Noble Metal
$225
D6740 Retainer Crown — Porcelain/
Ceramic
$295
D6750 Retainer Crown — Porcelain
Fused to High Noble Metal
$340
D6751 Retainer Crown — Porcelain
Fused to Predominantly Base
Metal
$295
D6752 Retainer Crown — Porcelain
Fused to Noble Metal
$295
D6753 Retainer Crown - Porcelain
Fused to Titanium and Titanium
Alloys
$295
D6780 Retainer Crown — 3/4 Cast
High Noble Metal
$340
D6781 Retainer Crown — 3/4 Cast
Predominantly Base Metal
$295
D6782 Retainer Crown — 3/4 Cast
Noble Metal
$295
D6783 Retainer Crown — 3/4
Porcelain/Ceramic
$295
D6784 Retainer Crown 3/4- Titanium
and Titanium Alloys
$295
D6790 Retainer Crown — Full Cast
High Noble Metal
$340
D6791 Retainer Crown — Full Cast
Predominantly Base Metal
$295
D6792 Retainer Crown — Full Cast
Noble Metal
$295
D6794 Retainer Crown — Titanium $340
Other Fixed Partial Denture Services
D6930 Recement Fixed Partial
Denture
$25
D6980 Fixed Partial Denture Repair
Necessitated by Restorative
Material Failure
$45
Codes
Description of
Covered Services Copayments
D7000-D7999 VIII. Oral and Maxillofacial Surgery
The following are covered services under Dental Tier
3 only.
Extractions Includes local anesthesia, suturing, if needed,
and routine post-operative care.
D7111 Extraction — Coronal
Remnants — Deciduous Tooth
$20
D7140 Extraction — Erupted Tooth or
Exposed Root (Elevation and/
or Forceps Removal) Includes
Removal of Tooth Structure,
Minor Smoothing of Socket
Bone, and Closure, as
Necessary
$35
Surgical Extractions Includes local anesthesia, suturing,
if needed, and routine post-operative care.
D7210 Extraction — Erupted Tooth
Requiring Removal of Bone
and/or Sectioning of Tooth,
and Including Elevation of
Mucoperiosteal Flap if Indicated
$45
D7220 Removal of Impacted Tooth —
Soft Tissue
$80
D7230 Removal of Impacted Tooth —
Partially Bony
$80
D7240 Removal of Impacted Tooth —
Completely Bony
$100
D7241 Removal of Impacted Tooth —
Completely Bony With
Complications
$100
Page 15 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
Codes
Description of
Covered Services Copayments
Surgical Extractions Includes local anesthesia, suturing,
if needed, and routine post-operative care.
D7250 Removal of Residual Tooth
Roots — Cutting Procedure
$45
D7251 Coronectomy — Intentional
Partial Tooth Removal
$48
Other Surgical Procedures
D7260 Oroantral Fistula Closure $150
D7261 Primary Closure of a Sinus
Perforation
$150
D7270 Tooth Reimplantation/
Stabilization
$90
D7280 Exposure of an Unerupted
Tooth
$90
D7282 Mobilization of Erupted or
Malpositioned Tooth to Aid
Eruption
$70
D7283 Placement of Device to
Facilitate Eruption of Impacted
Tooth
$25
D7285 Biopsy of Oral Tissue — Hard
(Bone, Tooth)
$95
D7286 Biopsy of Oral Tissue — Soft $40
D7287 Exfoliative Cytology — Sample
Collection
$13
D7291 Transseptal Fiberotomy Supra
Crestal Fiberotomy — By
Report
$35
Codes
Description of
Covered Services Copayments
Alveoloplasty — Surgical Preparation of the Ridge for
Dentures
D7310 Alveoloplasty in Conjunction
Wwith Extractions — Four or
More Teeth or Tooth Spaces,
per Quadrant.
The Alveoloplasty is Distinct
(Separate Procedure) from
Extractions. Usually in
Preparation for a Prosthesis
or Other Treatments Such as
Radiation Therapy and
Transplant Surgery
$45
D7311 Alveoloplasty in Conjunction
with Extractions — One to
Three Teeth or Tooth Spaces,
per Quadrant.
The Alveoloplasty is Distinct
(Separate Procedure) from
Extractions. Usually in
Preparation for a Prosthesis or
Other Treatments Such as
Radiation Therapy and Trans-
plant Surgery
$25
D7320 Alveoloplasty not in
Conjunction With Extractions
— Per Quadrant
$55
D7321 Alveoloplasty not in Conjunc-
tion with Extractions — One to
Three Teeth or Tooth Spaces
per Quadrant
$35
Removal of Cysts, Tumors, and Neoplasms
D7450 Removal of Benign Odontogen-
ic Cyst or Tumor — Lesion up
to 1.25 cm Diameter
$90
D7451 Removal of Benign Odonto-
genic Cyst or Tumor — Lesion
Greater than 1.25 cm Diameter
$90
D7460 Removal of Benign Non-Odon-
togenic Cyst or Tumor — Lesion
up to 1.25 cm Diameter
$90
Codes
Description of
Covered Services Copayments
D7461 Removal of Benign Non-Odon-
togenic Cyst or Tumor —
Lesion Greater than 1.25 cm
Diameter
$90
Excision of Bone Tissue
D7471 Removal of Lateral Exostosis
— Maxilla or Mandible
$135
D7472 Removal Torus Palatinus $135
D7473 Removal Torus Mandibularis $135
D7485 Reduction of Osseous
Tuberosity
$135
Surgical Incision
D7510 Incision and Drainage of
Abscess — Intraoral — Soft
Tissue
$40
D7511 Incision and Drainage of
Abscess — Intraoral — Soft
Tissue — Complicated
(Includes Drainage of Multiple
Facial Spaces)
$45
D7520 Incision and Drainage of
Abscess — Extraoral — Soft
Tissue
$55
D7521 Incision and Drainage of
Abscess — Extraoral — Soft
Tissue — Complicated
(Includes Drainage of Multiple
Facial Spaces)
$60
Other Repair Procedures
D7922 Placement of Intra-Socket
Bilolgical Dressing to Aid In
Hemostasis or Clot Stabiliza-
tion, Per Site
$0
D7953 Bone Replacement Graft for
Ridge Preservation — Per Site
$100
Retiree Dental Plans — Member Guidebook January 2024 Page 16
State Health Benets Program School Employees’ Health Benets Program
Codes
Description of
Covered Services Copayments
D7960 Frenulectomy — Also Known
as Frenectomy or Frenotomy
— Separate Procedure not
Incidental to Another Proce-
dure. Removal or Release of
Mucosal and Muscle Elements
of a Buccal, Labial, or Lingual
Frenum that is Associated
with a Pathological Condition,
or Interferes with Proper Oral
Development or Treatment
$90
D7963 Frenuloplasty $100
D7970 Excision of Hyperplastic Tissue
— Per Arch
$90
D7971 Excision of Pericoronal Gingiva
Removal of Inammatory or
Hypertrophied Tissues
Surrounding Partially Erupted/
Impacted Teeth
$45
D7972 Surgical Reduction of Fibrous
Tuberosity
$90
D9000-D9999 IX. Adjunctive General Services
The following are covered services under Dental Tier
3 only.
Miscellaneous Services
D9110 Palliative (Emergency) Treat-
ment of Dental Pain — Minor
Procedure
$15
D9211 Regional Block Anesthesia $5
D9212 Trigeminal Division Block
Anesthesia
$5
D9215 Local Anesthesia $5
D9219 Evaluation for Deep Sedation
or General Anesthesia
$0
Codes
Description of
Covered Services Copayments
D9223 Deep Sedation/General An-
esthesia — Each 15-Minute
Increment
$30
D9230 Analgesia, Anxiolysis,
Inhalation of Nitrous Oxide
$5
D9243 Intravenous Moderate (Con-
scious) Sedation/Analgesia —
Each 15-Minute Increment
$30
D9310 Consultation (Diagnostic
Service Provided by a Dentist
or Physician other than
Practitioner Providing
Treatment)
$5
D9311 Treating Dentist Consults with
a Medical Health Care
Professional Concerning
Medical Issues that May Aect
Patient’s Planned Dental
Treatment
$5
D9430 Oce Visit Observation $0
D9440 Oce Visit After Hours $0
D9610 Therapeutic Drug Injection —
By Report
$5
D9612 Therapeutic Parenteral Drug,
Two or more Administrations
Dierent Medications
$0
D9630 Drugs or Medicaments
Dispensed in the Oce for
Home Use
$5
D9910 Application of Desensitizing
Medication
$5
D9930 Treat Complications — By
Report
$5
D9932 Cleaning and Inspection of
Removable Complete Denture,
Maxillary
$0
D9933 Cleaning and Inspection of
Removable Complete Denture,
Mandibular
$0
Codes
Description of
Covered Services Copayments
D9934 Cleaning and Inspection of
Removable Partial Denture,
Maxillary
$0
D9935 Cleaning and Inspection of
Removable Partial Denture,
Mandibular
$0
D9940 Occlusal Guard — By Report $60
D9942 Repair and/or Reline of
Occlusal Guard
$35
D9943 Occlusal Guard Adjustment $8
D9951 Occlusal Adjustment — Limited $5
D9952 Occlusal Adjustment —
Complete
$90
D9997 Dental Case Management -
Patients With Special Health
Care Needs
$0
Page 17 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
More Expensive Services
A covered individual may elect a more expensive pro-
cedure than an appropriate procedure recommended
by the dentist. The covered individual shall pay any
copayment required for the less expensive procedure,
plus the dierence in cost between the two procedures,
on the basis of the reasonable and customary dental
charges for the procedures.
Emergency Services — Out of Area
Emergency Treatment is dened as when a covered
SHBP (or SEHBP) member or dependent is at least 50
miles from home, any necessary service or procedure
which is rendered as the direct result of an unforesee-
noccurrence and requires immediate, urgent action or
remedy. Examples are: acute pain, bleeding, fractured
tooth, broken lling, broken front tooth, broken denture,
and lost or loose crown. The reimbursement shall be at
the full amount of the charge up to a maximum of $100
per episode.
SERVICES NOT COVERED BY THE DPO
• A service started before the person became a cov-
ered individual under the plan.
• Replacement of lost, stolen, or damaged prostho-
dontic devices within two years of the date of initial
installation.
• A service not reasonably necessary for the dental
care of a covered individual or provided solely for
cosmetic purposes.
• Supplies of a type normally intended for home use,
such as toothpaste, toothbrushes, waterpicks, and
mouthwash.
• A service required because of war or an act of war.
• A service made available to a covered individual or
nanced by the federal, State, or local government.
This includes the federal Medicare program and
any similar federal program, any Workers’ Com-
pensation law or similar law, any automobile no-
fault law, or any other program or law under which
the covered individual is, or could be, covered. The
exclusion is applicable whether or not the covered
individual receives the service, makes a claim or
receives compensation for the service, or receives
a recovery from a third party for damages.
• A service not furnished by a dentist or physician
licensed to provide the dental service, except for
a service performed by a licensed dental hygienist
under the direction of a dentist.
• General anesthesia, except when medically nec-
essary in connection with covered oral and peri-
odontal surgery procedures.
• Hospitalization.
• Any dental implant including any crowns, prosthe-
ses, devices, or appliances attached to implants.
• Experimental procedures.
• Appliances, restorations, and procedures to alter
vertical dimension and/or restore occlusion, in-
cluding temporomandibular joint dysfunction, ex-
cept oral splints.
• Procedures that are not listed.
• A service covered under any medical, surgical,
or major medical plan (including a Health Mainte-
nance Organization — HMO) provided by the em-
ployer.
• Orthodontics.
• Services and supplies provided in connection with
treatment or care that is not covered under the
plan.
RETIREE DENTAL EXPENSE PLAN
The Retiree Dental Expense Plan (DEP) is a Prefered
Provider Organization (PPO) plan that will reimburse
you for a portion of the expenses you, and your en-
rolled eligible dependents, incur for dental care provid-
ed by dentists or physicians licensed to perform dental
services in the state in which they are practicing. Not
all dental services are eligible for reimbursement, and
some services are eligible only up to a limited amount.
Deductibles
Diagnostic and preventive services are not subject to
an annual deductible amount. For all other services an
annual deductible amount of $50 of covered expenses
that you or each of your dependents incur in a calendar
year is not eligible for reimbursement. However, if there
are three or more members of your family enrolled in
the plan, no additional deductibles are charged for the
calendar year after a total of $150 in eligible expens-
es. Charges incurred in a dental plan prior to your en-
rollment in this plan will not count towards your annual
deductible.
After any applicable annual deductible is satised, you
are reimbursed a percentage of the negotiated, dis-
counted fee for in-network services or reasonable and
customary allowance for out-of-network services that
are covered under the plan.
Discounted Fee-for-Service Network
It is recommended that you take advantage of a spe-
cial network of participating dental providers who dis-
count their fees for services. When you use a partic-
ipating dental provider, you only pay the provider any
applicable deductible and the appropriate coinsurance
based on the discounted fee, thereby reducing your
out-of-pocket cost. In most cases the participating
dental provider will submit the claims directly for you,
eliminating the necessity of your ling claim forms. Out-
Retiree Dental Plans — Member Guidebook January 2024 Page 18
State Health Benets Program School Employees’ Health Benets Program
of-network dentists are not required to le claims on
your behalf, and you may be responsible for submitting
a claim form directly to Aetna. In some cases an out-
of-network dentist may ask you to pay your bill in full
and ask you to submit the claim for reimbursement. To
nd out if your provider participates in the discounted
network, contact Aetna, toll-free, at: 1-877-STATENJ
(1-877-782-8365), or visit the Aetna website at:
www.aetna.com/docnd/custom/statenj
Reasonable and Customary Allowance
The reasonable and customary allowance only applies
to out-of-network services. When utilizing an out-of-
network provider, the plan covers only that part of a
provider’s fee for a service or supply that is reasonable
and customary. Generally speaking, a fee charged by
your dentist, or by any other provider of services or
supplies, is considered reasonable and customary if it
doesn’t exceed the prevailing fee charged for the same
service or supply by similar providers in the same geo-
graphic area. The prevailing allowance used for this
plan is provided by Ingenix (a national database of den-
tal plan services and fees) and may dier from the actu-
al amount your dentist charges. If your dentist charges
more than the reasonable and customary allowance,
you are responsible for the amount above the reason-
able and customary allowance unless a participating
dental provider is used.
Reimbursement
Once members meet their $50 annual deductible (if ap-
plicable), the costs of all other eligible services for that
person are reimbursed at a percentage of the reason-
able and customary allowance for the service.
Annual Benet Maximum
The most the plan will pay for any one person in any
calendar year is $1,500. This maximum applies to all
eligible services.
PLAN DESIGN
Three Tier Benet Design
The Retiree DEP features three benet tiers (see the
“Retiree Dental Expense Plan Reimbursement Tiers”
chart). Your initial benet tier depends upon whether
you were covered under a group dental plan just prior
to your enrollment:
• If you, the retiree, were covered under a group
dental plan for at least one year within 60 days
of joining this plan, you and your eligible depen-
dents will be enrolled at the highest level of bene-
ts — Tier 3. Specic information concerning the
12-month dental plan enrollment must be provided
on your enrollment application.
• If you, the retiree, were not covered under a group
dental plan for at least one year within 60 days of
joining this plan, you and your eligible dependents
will be enrolled at the lowest level of reimburse-
ment — Tier 1. Each year you remain a member of
the plan, your reimbursement benet will rise to a
higher tier until you are at the top level of benets
(Tier 3).
COVERED SERVICES
The Retiree DEP covers preventive care, basic ser-
vices, and major restorative services at dierent levels.
The deductible is waived for preventive care. The Re-
tiree DEP does not reimburse for any orthodontic ser-
vices. A general description of each category of service
follows.
Preventive Care
Preventive care consists of diagnostic and preventive
services that are precautionary services intended to
maintain oral health and reduce the eects of tooth
decay or gum disease that could lead to an increased
need for more costly restorative services. They include
the following:
• Oral evaluations (includes comprehensive, period-
ic, and problem-focused oral evaluations);
• X-rays (limitations apply - see the “DEP Services
Eligible for Reimbursement” section);
• Prophylaxis (cleaning of the teeth, including the
removal of plaque, calculus, and stains from tooth
structures, limitations apply - see the “DEP Ser-
vices Eligible for Reimbursement” section);
• Fluoride Treatments (topical application of uoride
for children under age 19); and
• Laboratory and other dental diagnostic tests.
Basic Services
Basic services include:
• Emergency Treatment (Palliative only);
• Space Maintainers (i.e., passive appliances - can
be xed or removable);
• Simple Extractions;
• Surgical Extractions;
• Oral Surgery;
• Anesthesia Services;
• Basic Restorations (i.e., amalgam restorations and
resin-based composite restorations);
• Endodontics (i.e., treatment of diseases of the den-
tal pulp, including root canal and associated thera-
py); and
• Repairs to removable and xed dentures.
Page 19 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
Major Restorative Services
Major restorative services include those services that
restore existing teeth. These services are utilized only
if a tooth cannot be restored with an amalgam, acrylic,
synthetic porcelain, or composite lling restoration. In-
lays, onlays, and crowns are typical examples of major
restorative services.
Other Major Restorative services include:
• Periodontal services include those services in-
volving the maintenance, reconstruction, regener-
ation, and treatment of the supporting structures
surrounding teeth, including bone, gum tissue, and
root surfaces.
• Prosthodontic services include both removable
and xed dentures (bridges) replacing missing
teeth.
Note: Orthodontic services are not covered under the
Retiree DEP.
ADDITIONAL PROVISIONS OF THE PLAN
How Payments Are Made
If you use a participating dental network provider, pay-
ments are made directly to the provider less any appli-
cable deductible or appropriate coinsurance based on
the discounted fee (see the “Deductibles” section).
If you use a non-participating provider, the provider
may ask you to pay for the service in advance. If the
provider’s oce asks you to pre-pay for the services, it
will be your responsibility to submit the claim to Aetna
for reimbursement. The retiree may, however, authorize
Aetna to send the reimbursement directly to the dental
provider by completing the appropriate section of the
claim form. Additionally, whenever a law or court order
requires the payment of dental expense benets under
the plan to be made to a person or facility other than
the retiree, the payment will be made to that person or
facility upon proper notication (letter and a copy of the
order/law).
RETIREE DENTAL EXPENSE PLAN REIMBURSEMENT TIERS
Annual
Deductible Coinsurance
Maximum
Annual
Benet
Tier 1 $50 per person,
but not more than
$150 total; waived
for Preventive Care
IN-NETWORK
80% - Preventive &
Diagnostic Care
50% - Basic Restorative
30% - Major Restorative
OUT-OF-NETWORK
70% - Preventive &
Diagnostic Care
50% - Basic Restorative
20% - Major Restorative
$1,500
per person
Tier 2 $50 per person,
but not more than
$150 total; waived
for Preventive Care
IN-NETWORK
90% - Preventive &
Diagnostic Care
60% - Basic Restorative
40% - Major Restorative
OUT-OF-NETWORK
80% - Preventive &
Diagnostic Care
50% - Basic Restorative
30% - Major Restorative
$1,500
per person
Tier 3 $50 per person,
but not more than
$150 total; waived
for Preventive Care
IN-NETWORK
100% - Preventive Care
70% - Basic Restorative
50% - Major Restorative
OUT-OF-NETWORK
90% - Preventive &
Diagnostic Care
50% - Basic Restorative
40% - Major Restorative
$1,500
per person
Retiree Dental Plans — Member Guidebook January 2024 Page 20
State Health Benets Program School Employees’ Health Benets Program
Filing Deadline — Proof of Loss
Aetna must be given written proof that a dental service
has been performed for which a claim is made under
the coverage. This proof must cover the occurrence,
character, and extent of the service. It must be fur-
nished within 27 months of the date of service. For ex-
ample, if a service were incurred on February 1, 2017,
you would have until April 30, 2019, to le the claim.
A claim will not be considered valid unless proof of
the service is furnished within the time limit indicated
above. If it is not possible for you to provide proof within
the time limit, the claim may be considered valid upon
appeal if the reason the proof was not provided in a
timely basis was reasonable.
Itemized Bills Are Necessary
You must obtain itemized bills from the providers of ser-
vices for all dental expenses. The itemized bills must
include the following:
• Name and address of provider;
• Provider’s tax identication number;
• Name of patient;
• Subscriber’s identication number;
• Date of service;
• Type of service;
• Procedure code; and
• Charge for each service.
Predetermination of Benets
Predetermination is voluntary and allows you to know
what services are covered and what payments will be
made for treatment before the work is done. If you or
one of your dependents are likely to incur dental ex-
penses over $300, it is strongly recommended that you
ask your dentist to le for predetermination of benets.
This feature of the Retiree DEP ensures that both you
and the dentist will know in advance what part of the
dentist’s charges the plan will pay. If possible, treat-
ment should be completed within 90 days of receiving
the approved predetermination.
The predetermination of benets provision of the Re-
tiree DEP is important, because under the alternative
procedures provision (see the “Alternative Procedures”
section), Aetna has the right to pay the reasonable and
customary allowance for the method of treatment that
is proper and is economically sound.
How Predetermination of Benets Works — Your
dentist submits a treatment plan and Aetna determines
the amount the Retiree DEP will pay, and informs you
and the dentist of its payment decision. You and your
dentist should discuss the payment before the work is
started.
Predetermination of benets will help you avoid sur-
prises. Most dentists are familiar with predetermi-
nation procedures; if not, they should call Aetna at
1-877-STATENJ (1-877-782-8365). If your dentist sub-
mits a treatment plan for predetermination of benets
and then alters the course of treatment, Aetna will
adjust its payments accordingly. If the dentist makes
a major change in the treatment plan, a revised plan
should be sent.
Alternative Procedures
Usually there are several ways to treat a particular den-
tal problem. Payment will be based on the least costly
treatment so long as the result meets acceptable den-
tal standards. If you and the dentist decide you want a
more costly treatment method, you are responsible for
the charges beyond those for the less costly, appropri-
ate treatment.
DEP SERVICES
ELIGIBLE FOR REIMBURSEMENT
See the Glossary for a denition of terms.
• Oral evaluations covered at 80, 90, or 100 per-
cent in-network, or at 70, 80, or 90 percent out-
of-network depending on your benet tier (limited
to twice in a calendar year). Emergency or limited
oral evaluations are covered, limited to one evalua-
tion per patient, per year. Periodontal maintenance
evaluations are included as oral evaluations.
• X-rays (horizontal bitewing X-rays limited to two
series of up to four lms in a calendar year; ver-
tical bitewing X-rays limited to two series of up to
eight lms in a calendar year; set of full mouth or
panoramic X-rays limited to once per 36 month in-
terval; no more than 18 lms per set of full mouth
periapical X-rays).
• Oral prophylaxis, including the removal of plaque,
calculus, and stains from tooth structures (not in-
cluding scaling performed by a periodontist) and
polishing (limited to twice in a calendar year).
• Topical application of uoride for children under
age 19 limited to twice in a calendar year.
• Prosthodontic procedures (the replacement of an
existing xed or removable prosthetic appliance
is covered only after a ve-year period, measured
from the date on which the appliance was previ-
ously placed).
• Periodontics procedures (reimbursement for peri-
odontal surgical procedures, usually provided for
a specic quadrant, is limited to one surgical-type
procedure, per quadrant every 36 months). Reim-
bursement for periodontal scaling and root planing
procedures per specic quadrant is limited to one
procedure in a 12-month interval.
Page 21 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
• Periodontal surgical procedures, usually provided
for specic quadrants, are subject to a reduced re-
imbursement when the number of diseased teeth
in a quadrant are less than four. Additional reduc-
tion in benets may apply, when multiple types of
procedures are provided in the same quadrant, at
the same appointment.
• Restorative procedures, including llings, inlays,
onlays, and crowns (the replacement of a crown
is covered only after a ve-year period measured
from the date on which the crown was previously
placed).
• Emergency palliative treatment.
• Routine extractions of teeth.
• Endodontic services, such as pulpotomy and root
canal therapy.
• Space maintainers (other than for orthodontic
treatment).
• Oral surgical procedures considered dental in
nature — such as, but not limited to: surgical ex-
tractions, treatment of fractures, removal of lesions
of the mouth, and alveolectomy.
• Apicoectomy.
• General anesthesia (including conscious sedation
coverage) when medically necessary and in con-
nection with covered oral and periodontal surgical
procedures.
DEP SERVICES NOT
ELIGIBLE FOR REIMBURSEMENT
• Any orthodontic service.
• Gold restorations other than crowns, inlays, and
onlays.
• Any service or item not reasonably necessary for
the dental care of the patient.
• Endosteal, subperiosteal, and transosteal tooth
implants.
• Protective devices such as athletic mouth guards.
• Plaque control.
• Myofunctional therapy.
• A charge in connection with appliances, resto-
rations, or procedures needed to alter vertical di-
mensions or restore occlusion, or for the purpose
of splinting or correcting attrition, abrasion, or ero-
sion.
• Crowns, inlays, or onlays if used in splinting proce-
dures during periodontal treatment.
• Charges for sterilization or asepsis.
• A service for cosmetic purposes.
• Any charge for a supply that is normally for home
use such as toothpaste, toothbrushes, water-pick,
or mouthwash.
• A dental examination when required as a condi-
tion of employment by an employer, a government
agency, or the terms of a labor agreement.
• Charges for services not reasonably necessary to
produce a professionally acceptable result.
• A service or supply due to a war or any act of war.
• A service not furnished by a dentist or physician
licensed to provide the dental service, except for
a service performed by a licensed dental hygienist
under the direction of a dentist.
• A service rendered by a provider that is beyond the
scope of the provider’s license.
• A charge made by a dentist for a failure of the pa-
tient to keep an appointment.
• A charge for the completion of any claim forms.
• A charge in connection with any procedure started
before the patient was eligible for reimbursement
in this plan; except that a procedure will not have
been considered to have started with an oral pro-
phylaxis or a diagnostic procedure.
• Any service or supply which is furnished or made
available to a patient or nanced by federal, State,
or local government, including Medicare or a like
plan, Workers’ Compensation law or a similar law,
any automobile no-fault law, or any other plan or
law under which the patient is or could be covered,
whether or not the patient makes any claim or re-
ceives compensation under it.
• Any charge incurred after the patient is no longer
covered, except in the case of an extension of cov-
erage (see the “Extension of Coverage Provisions”
section).
• Any charge for a service that is more than the rea-
sonable and customary allowance (see the “Rea-
sonable and Customary Allowance” section).
• Any charge for a service rendered by a member of
the patient’s immediate family (including you, your
spouse/partner, your child, brother, sister, or par-
ent of you or your spouse/partner).
• Any service or supply other than those specically
covered under this program.
• Services and supplies provided in connection with
treatment or care that is not covered under the
plan.
Retiree Dental Plans — Member Guidebook January 2024 Page 22
State Health Benets Program School Employees’ Health Benets Program
APPENDIX I
CLAIM APPEAL PROCEDURES
You or your authorized representative may appeal and
request that the dental plan reconsider any claim or
any portion(s) of a claim for which you believe bene-
ts have been erroneously denied based on the plan’s
limitations and/or exclusions. This appeal may be of an
administrative or dental nature. Administrative appeals
might question eligibility or plan benet decisions such
as whether a particular service is covered or paid ap-
propriately. Dental appeals refer to the determination of
dental need, appropriateness of treatment, or experi-
mental and/or investigational procedures.
The following information must be given at the time of
each inquiry:
• Name(s) and address(es) of patient and
employee;
• Employee’s identication number;
• Date(s) of service(s);
• Provider’s name and identication number;
• The specic remedy being sought; and
• The reason you think the claim should be
reconsidered.
If you have any additional information or evidence
about the claim that was not given when the claim was
rst submitted, be sure to include it.
If dissatised with a nal health plan decision on a
dental appeal, only the member or the member’s le-
gal representative (this does not include the provider
of service) may appeal, in writing, to the State Health
Benets Commission. If the member is deceased or in-
capacitated, the individual legally entrusted with their
aairs may act on the member’s behalf. Request for
consideration must contain the reason for the disagree-
ment along with copies of all relevant correspondence
and should be directed to the following address:
Appeals Coordinator
State Health Benets Commission
P.O. Box 299
Trenton, NJ 08625-0299
Notication of all Commission decisions will be made in
writing to the member. If the Commission approves the
member’s appeal, the decision is binding upon the den-
tal plan. If the Commission denies the member’s ap-
peal, the member will be informed of further steps that
may be taken in the denial letter from the Commission.
Any member who disagrees with the Commission’s
decision may request, within 45 days in writing to the
Commission, that the case be forwarded to the Oce
of Administrative Law (OAL). The Commission will then
determine if a factual hearing is necessary. If so the
case will be forwarded to the OAL. An Administrative
Law Judge (ALJ) will hear the case and make a recom-
mendation to the Commission, which the Commission
may adopt, modify, or reject. If the recommendation is
rejected, the administrative appeal process is ended.
When the administrative process is ended, further ap-
peals may be made to the Superior Court of New Jer-
sey, Appellate Division.
If your case is forwarded to the OAL, you will be re-
sponsible for the presentation of your case and for
submitting all evidence. You will be responsible for any
expenses involved in gathering evidence or material
that will support your grounds for appeal. You will be
responsible for any court ling fees or related costs that
may be necessary during the appeal’s process. If you
require an attorney or expert dental testimony, you will
be responsible for any fees or costs incurred.
HIPAA PRIVACY
The Retiree Dental Plans make every eort to safe-
guard the dental information of their members and
complies with the privacy provisions of the federal
Health Insurance Portability and Accountability Act (HI-
PAA) of 1996. HIPAA requires health plans to maintain
the privacy of any personal information relating to its
members’ physical or mental health. See Appendix III
(on page 27) for the SHBP/SEHBP’s Notice of Privacy
Practices.
AUDIT OF DEPENDENT COVERAGE
Periodically the NJDPB performs an audit using a ran-
dom sample of members to determine if enrolled de-
pendents are eligible under plan provisions. Proof of
dependency such as a marriage, civil union, or birth
certicates, or tax returns are required. Coverage for
ineligible dependents will be terminated. Failure to
respond to the audit will result in the termination of
all coverage and may include nancial restitution for
claims paid. Members who are found to have intention-
ally enrolled an ineligible person for coverage will be
prosecuted to the fullest extent of the law.
HEALTH CARE FRAUD
Health care fraud is an intentional deception or misrep-
resentation that results in an unauthorized benet to a
member or to some other person. Any individual who
willfully and knowingly engages in an activity intended
to defraud the SHBP or SEHBP will face disciplinary
action that could include termination of employment
and may result in prosecution. Any member who re-
ceives monies fraudulently from a health plan will be
required to fully reimburse the plan.
Page 23 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
APPENDIX II
GLOSSARY
Alveolectomy — Surgical excision of a portion of the
dentoalveolar process, for recontouring the
tooth socket ridge at the time of tooth remov-
al in preparation for a dental prosthesis (den-
ture).
Amalgam — An alloy used in dental restoration.
Apicoectomy — Surgical removal of a dental root
apex. Root resection.
Bitewing X-Ray — X-rays taken with the lm holder
held between the teeth and the lm parallel to
the teeth.
Coinsurance — The percentage of the eligible charge
that the retiree/member must pay.
Crown — That part of a tooth that is covered with
enamel or an articial substitute for that part.
Deductible — The rst eligible expense, or portion
thereof, incurred within each calendar year
that the member is required to pay before re-
imbursement for eligible expenses begins.
Endodontics — Concerned with the biology and pa-
thology of the dental pulp and surrounding tis-
sues. Root canal treatment.
Inlay — A cast metallic or ceramic lling for a dental
cavity.
Member — With respect to the Retiree Dental Plans,
retirees and any dependents who are eligible
to enroll in the SHBP/SHEHBP.
Member Identication Card — A wallet-sized, plas-
tic card issued by your plan that identies the
retiree/dependent named thereon as a plan
member.
Onlay — A type of metal restoration that overlays the
tooth to provide additional strength to that
tooth.
Palliative Treatment — Alleviation of symptoms with-
out curing the underlying disease.
Periodontics — Concerned with the treatment of ab-
normal conditions and diseases of the tissues
that surround and support the teeth.
Prophylaxis — A series of procedures whereby cal-
culus (calcied deposits), stain, and other ac-
cretions are removed from the clinical crowns
of the teeth and the enameled surfaces are
polished.
Prosthodontics — The science and art of providing
suitable substitutes for crowns of teeth, or for
replacing lost or missing teeth.
Resin — A material used in dental restoration.
Scaling and Root Planing — The removal of subgingi-
val calcied deposits around the teeth and the
cleaning of the gingival pocket.
State Health Benets Commission (Commission)
— The entity created by N.J.S.A. 52:14-17.27
and charged with the responsibility of over-
seeing the State Health Benets Program.
APPENDIX III
NOTICE OF PRIVACY PRACTICES TO ENROLL-
EES
State Health Benets Program
School Employees’ Health Benets Program
This Notice describes how medical
information about you may be used
and disclosed and how you can get
access to this information.
Please review it carefully.
Protected Health Information
The State Health Benets Program and School Em-
ployees’ Health Benets Program (Programs) are re-
quired by the federal Health Insurance Portability and
Accountability Act (HIPAA) and State laws to main-
tain the privacy of any information that is created or
maintained by the Programs that relates to your past,
present, or future physical or mental health. This Pro-
tected Health Information (PHI) includes information
communicated or maintained in any form. Examples
of PHI are your name, address, Social Security num-
ber, birth date, telephone number, fax number, dates
of health care service, diagnosis codes, and procedure
codes. PHI is collected by the Programs through var-
ious sources, such as enrollment forms, employers,
health care providers, federal and State agencies, or
third-party vendors.
The Programs are required by law to abide by the
terms of this Notice. The Programs reserve the right to
change the terms of this Notice. If material changes are
made to this Notice, a revised Notice will be sent.
Retiree Dental Plans — Member Guidebook January 2024 Page 24
State Health Benets Program School Employees’ Health Benets Program
Uses and Disclosures of PHI
The Programs are permitted to use and to disclose
PHI in order for our members to obtain payment for
health care services and to conduct the administrative
activities needed to run the Programs without specic
member authorization. Under limited circumstances,
we may be able to provide PHI for the health care oper-
ations of providers and health plans. Specic examples
of the ways in which PHI may be used and disclosed
are provided below. This list is illustrative only and not
every use and disclosure in a category is listed.
• The Programs may disclose PHI to a doctor or a
hospital to assist them in providing a member with
treatment.
• The Programs may use and disclose member PHI
so that our Business Associates may pay claims
from doctors, hospitals, and other providers.
• The Programs receive PHI from employers, includ-
ing the member’s name, address, Social Security
number, and birth date. This enrollment informa-
tion is provided to our Business Associates so that
they may provide coverage for health care benets
to eligible members.
• The Programs and/or our Business Associates
may use and disclose PHI to investigate a com-
plaint or process an appeal by a member.
• The Programs may provide PHI to a provider, a
health care facility, or a health plan that is not our
Business Associate that contacts us with ques-
tions regarding the member’s health care cover-
age.
• The Programs may use PHI to bill the member for
the appropriate premiums and reconcile billings
we receive from our Business Associates.
• The Programs may use and disclose PHI for fraud
and abuse detection.
• The Programs may allow use of PHI by our Busi-
ness Associates to identify and contact our mem-
bers for activities relating to improving health or
reducing health care costs, such as information
about disease management programs or about
health-related benets and services, or about
treatment alternatives that may be of interest to
them.
• In the event that a member is involved in a lawsuit
or other judicial proceeding, the Programs may
use and disclose PHI in response to a court or ad-
ministrative order as provided by law.
• The Programs may use or disclose PHI to help
evaluate the performance of our health plans. Any
such disclosure would include restrictions for any
other use of the information other than for the in-
tended purpose.
• The Programs may use PHI in order to conduct an
analysis of our claims data. This information may
be shared with internal departments such as audit-
ing or it may be shared with our Business Associ-
ates, such as our actuaries.
Except as described above, unless a member speci-
cally authorizes us to do so, the Programs will provide
access to PHI only to the member, the member’s au-
thorized representative, and those organizations who
need the information to aid the Programs in the con-
duct of its business (our “Business Associates”). An
authorization form may be obtained on our website at:
www.nj.gov/treasury/pensions or by sending an
email to: hipaaform@treas.nj.gov A member may re-
voke an authorization at any time.
Restricted Uses
• PHI that contains genetic information is prohibited
from use or disclosure by the Programs for under-
writing purposes.
• The use or disclosure of PHI that includes psy-
chotherapy notes requires authorization from the
member.
When using or disclosing PHI, the Programs will make
every reasonable eort to limit the use or disclosure
of that information to the minimum extent necessary to
accomplish the intended purpose. The Programs main-
tain physical, technical, and procedural safeguards that
comply with federal law regarding PHI. In the event of
a breach of unsecured PHI the member will be notied.
Member Rights
Members of the Program have the following rights re-
garding their PHI.
Right to Inspect and Copy: With limited exceptions,
members have the right to inspect and/or obtain a copy
of their PHI that the Programs maintain in a designated
record set, which consists of all documentation relating
to member enrollment and the Programs’ use of this
PHI for claims resolution. The member must make a
request in writing to obtain access to their PHI. The
member may use the contact information found at the
end of this Notice to obtain a form to request access.
Right to Amend: Members have the right to request
that the Programs amend the PHI that we have created
and that is maintained in our designated record set.
We cannot amend treatment records, or any other in-
formation created by others. To amend treatment re-
cords, a member must contact the treating physician,
facility, or other provider that created and/or maintains
these records.
Page 25 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
The Programs may deny the member’s request if: 1) we
did not create the information requested on the amend-
ment; 2) the information is not part of the designated
record set maintained by the Programs; 3) the member
does not have access rights to the information; or 4) we
believe the information is accurate and complete. If we
deny the member’s request, we will provide a written
explanation for the denial and the member’s rights re-
garding the denial.
Right to an Accounting of Disclosures: Members
have the right to receive an accounting of the instanc-
es in which the Program or our Business Associates
have disclosed member PHI. The accounting will re-
view disclosures made over the past six years. We will
provide the member with the date on which we made a
disclosure, the name of the person or entity to whom
we disclosed the PHI, a description of the information
we disclosed, the reason for the disclosure, and certain
other information. Certain disclosures are exempted
from this requirement (e.g., those made for treatment,
payment or health benets operation purposes, or
made in accordance with an authorization) and will not
appear on the accounting.
Right to Request Restrictions: The member has the
right to request that the Programs place restrictions on
the use or disclosure of their PHI for treatment, pay-
ment, or health care operations purposes. The Pro-
grams are not required to agree to any restrictions and
in some cases will be prohibited from agreeing to them.
However, if we do agree to a restriction, our agreement
will always be in writing and signed by the Privacy Of-
cer. The member request for restrictions must be in
writing. A form can be obtained by using the contact
information found at the end of this Notice.
Right to Restrict Disclosure: The member has the
right to request that a provider restrict disclosure of PHI
to the Programs or Business Associates if the PHI re-
lates to services or a health care item for which the in-
dividual has paid the provider in full. If payment involves
a exible spending account or health savings account,
the individual cannot restrict disclosure of information
necessary to make the payment but may request that
disclosure not be made to another program or health
plan.
Right to Receive Notication of a Breach: Members
have the right to receive notication in the event that
the Programs or a Business Associate discover unau-
thorized access or release of PHI through a security
breach.
Right to Request Condential Communications:
Members have the right to request that the Programs
communicate with them in condence about their PHI
by using alternative means or an alternative location,
if the disclosure of all or part of that information to an-
other person could endanger them. We will accommo-
date such a request if it is reasonable, if the request
species the alternative means or locations, and if it
continues to permit the Programs to collect premiums
and pay claims under the health plan.
To request changes to condential communications,
members must make their request in writing and must
clearly state that the information could endanger them
if it is not communicated in condence as they request-
ed.
Right to Receive a Paper Copy of the Notice: Mem-
bers are entitled to receive a paper copy of this Notice.
Please contact us using the information at the end of
this Notice.
Questions and Concerns
If you have questions or concerns, please contact the
Programs using the information listed at the end of this
notice.
If members think the Programs may have violated their
privacy rights, or they disagree with a decision made
about access to their PHI, in response to a request
made to amend or restrict the use or disclosure of their
information, or to have the Programs communicate with
them in condence by alternative means or at an al-
ternative location, they must submit their complaint in
writing. To obtain a form for submitting a complaint, use
the contact information below.
Members also may submit an online complaint to the
U.S. Department of Health and Human Services, at:
www.hhs.gov/hipaa/ling-a-complaint
The Programs support member rights to protect the pri-
vacy of PHI. It is your right to le a complaint with the
Programs or with the U.S. Department of Health and
Human Services.
Contact Oce:
New Jersey Division of Pensions & Benets
HIPAA Privacy Ocer
Address:
New Jersey Division of Pensions & Benets
Bureau of Policy and Planning
P.O. Box 295
Trenton, NJ 08625-0295
Email: [email protected]v
Retiree Dental Plans — Member Guidebook January 2024 Page 26
State Health Benets Program School Employees’ Health Benets Program
APPENDIX IV
PARTICIPATING RETIREE DENTAL PLANS
Plan Name
Web Addresses and Membership
Services Phone Number
Aetna DMO www.aetna.com/statenj
1-877-STATENJ (1-877-782-8365)
Cigna Dental Health, Inc. www.cigna.com/sites/stateofnjdental
1-800-564-7642
Horizon Dental Choice www.horizonblue.com
1-800-433-6825
MetLife www.metlife.com/dental
1-866-880-2984
Dental Expense Plan
(PPO Administered by Aetna)
www.aetna.com/statenj
1-877-STATENJ (1-877-782-8365)
Page 27 January 2024 Retiree Dental Plans — Member Guidebook
School Employees’ Health Benets Program State Health Benets Program
HEALTH BENEFITS CONTACT INFORMATION
Addresses
Our Mailing Address is:
New Jersey Division of Pensions & Benets
Health Benets Bureau
P.O. Box 299
Trenton, NJ 08625-0299
Our website address is:
www.nj.gov/treasury/pensions
Our Email Address is:
pensions.nj@treas.nj.gov
Telephone Numbers
Division of Pensions & Benets
Oce of Client Services .............. (609) 292-7524
Relay Operator (Hearing Impaired) .. Dial 711 and
provide operator with: .................(609) 292-6683
New Jersey State Police
Oce of Employer and
Organization Development .........1-800-367-6577
New Jersey Department of Banking and Insurance
Individual Health Coverage
Program Board ........................... 1-800-838-0935
Consumer Assistance for
Health Insurance .......................... (609) 292-5316
Independent Health Care
Appeals Program ........................1-800-466-7467
New Jersey Department of Human Services
Pharmaceutical Assistance to the
Aged and Disabled (PAAD) ........1-800-792-9745
Division on Senior Aairs ............1-800-792-8820
Insurance Counseling .................1-800-792-8820
Centers for Medicare and Medicaid Services
New Jersey Medicare —
Part A and Part B ....................1-800-MEDICARE
HEALTH BENEFITS PUBLICATIONS
Publications and fact sheets available from the NJD-
PB provide information on a variety of subjects. Fact
sheets, guidebooks, applications, and other publica-
tions are available for viewing or downloading on our
website.
General Publications
Summary Program Description — An overview of
SHBP/SEHBP eligibility and plans
Plan Design Comparison Charts — Out-of-pocket cost
comparison charts for State employees, local govern-
ment employees, local education employees, and all
retirees
Health Benet Fact Sheets
• Health Benets Coverage — Enrolling as a Retir-
ee
• Health Benet Programs and Medicare Parts A &
B for Retirees
• COBRA — The Continuation of Health Benets
• Health Benets Benets Retired Coverage under
Chapter 330
• Family Status Changes - Employees
• Family Status Changes - Retirees
• Health Benets Coverage Continuation for Over-
age Children With Disabilities
• Dental Plans — Retirees
• Health Benets Coverage of Children until Age 31
under Chapter 375, P.L. 2007
• Civil Unions and Domestic Partnerships
Health Plan Member Guidebooks
• NJ DIRECT/CWA Unity DIRECT Member Guide-
book
• Horizon HMO Member Guidebook
• Horizon OMNIA Member Guidebook
• NJ DIRECT HDHP Member Guidebook
• Prescription Drug Plans Member Guidebook
• Employee Dental Plans Member Guidebook
• Retiree Dental Plans Member Guidebook
