234
Proc.
roy.
Soc.
Med.
Volume
61
March
1968
8
.i:
...........s
:~~~~~~~~~~~~~~~~~~~~~~~~~~
.. ..
:..........
Fig
I1I
Thoracopagus
Fig
12
Monozygotic
twins,
one
acardiac.
There
is
only
rudimentary
cephalic
development,
there
are
no
upper
limbs
and
the
lower
limbs
are
fused.
The
co-twin
on
the
left
is
normal/v
developedfor
19
weeks
gestation
30
%
of
the
tissue
relating
to
the
twin
on
the
right,
who
weighed
1,700
g;
his
partner
weighed
2,700
g,
a
discrepancy
presumably
due
to
the
relatively
poor
placental
supply
of
the
underweight
twin.
Our
survey
has
shown
many
such.
examples,
though
there
are
exceptions.
Monoamniotic
twins
have
the
highest
foetal
mortality
but
the
reason
is
not
clear;
one
cause
in
our
series
is
entanglement
of
the
two
cords
(Wharton
et
aL.
1968).
All
conjoined
twins
are
of
course
monoamniotic.
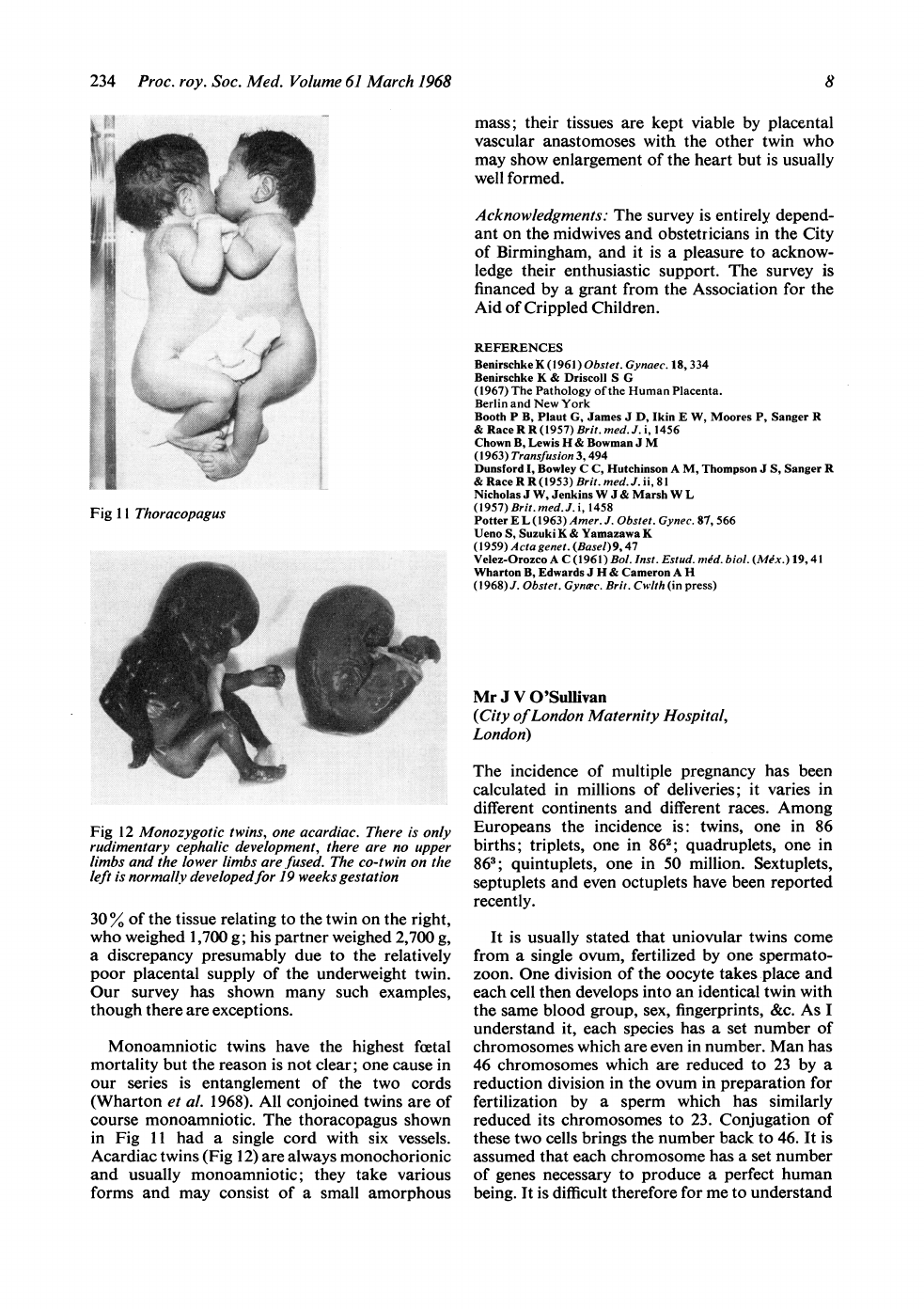
The
thoracopagus
shown
in
Fig
11I
had
a
single
cord
with
six
vessels.
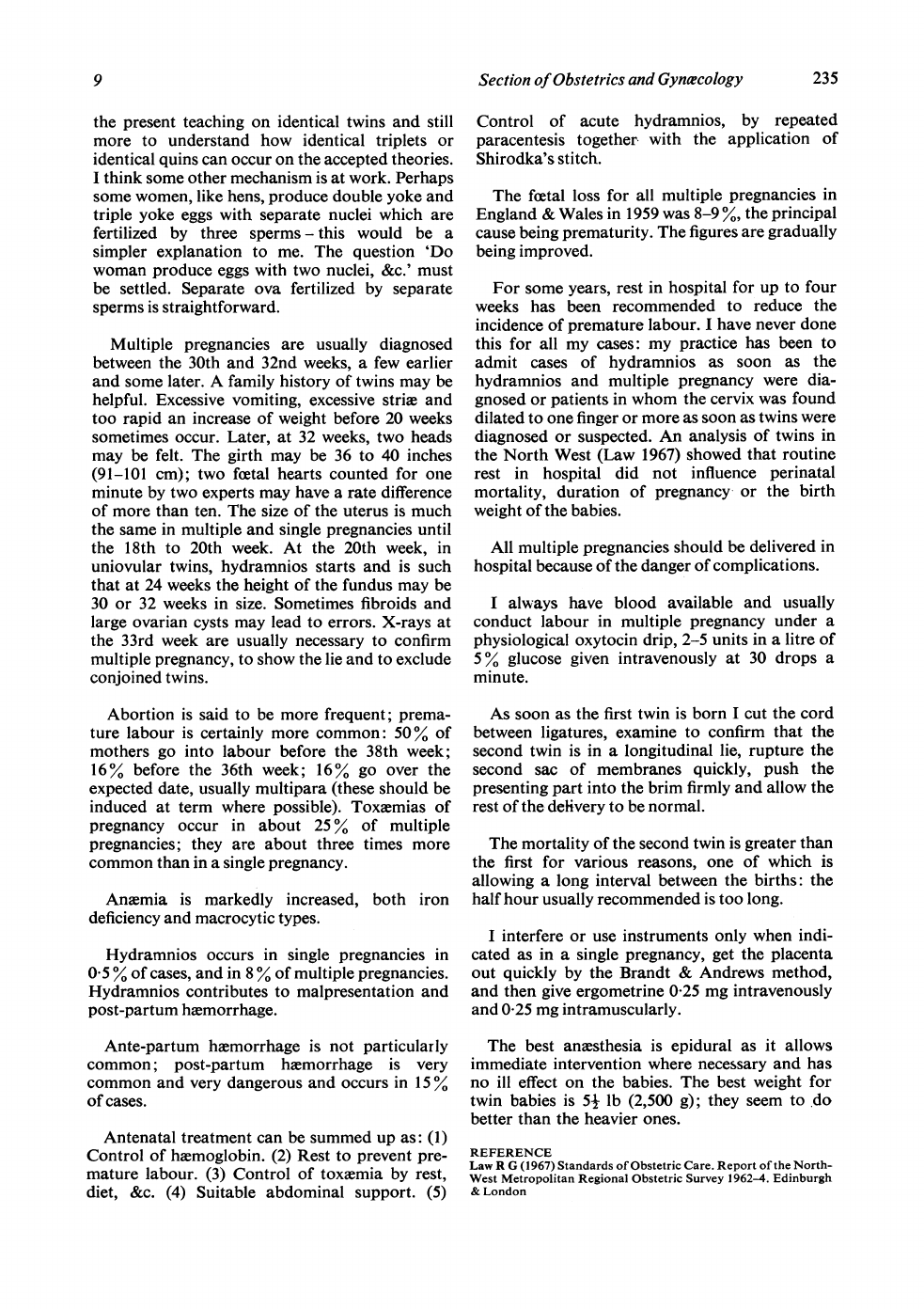
Acardiac
twins
(Fig
12)
are
always
monochorionic
and
usually
monoamniotic;
they
take
various
forms
and
may
consist
of
a
small
amorphous
mass;
their
tissues
are
kept
viable
by
placental
vascular
anastomoses
with
the
other
twin
who
may
show
enlargement
of
the
heart
but
is
usually
well
formed.
Acknowledgments:
The
survey
is
entirely
depend-
ant
on
the
midwives
and
obstetricians
in
the
City
of
Birmingham,
and
it
is
a
pleasure
to
acknow-
ledge
their
enthusiastic
support.
The
survey
is
financed
by
a
grant
from
the
Association
for
the
Aid
of
Crippled
Children.
REFERENCES
Benirschke
K
(1961)
Obstet.
Gynaec.
18,
334
Benirschke
K
&
Driscoll
S
G
(1967)
The
Pathology
of
the
Human
Placenta.
Berlin
and
New
York
Booth
P
B,
Plaut
G,
James
J
D,
Ikin
E
W,
Moores
P,
Sanger
R
&
RaceR
R(1957)Brit.med.J.i,
1456
Chown
B,
Lewis
H
&
Bowman
J
M
(1963)
Transfusion
3,
494
Dunsford
I,
Bowley
C
C,
Hutchinson
A
M,
Thompson J
S,
Sanger
R
&
Race
R
R
(1953)
Brit.
med.
J.
ii,
81
Nicholas
J
W,
Jenkins
W
J
&
Marsh
W
L
(1957)
Brit.
med.J.
i,
1458
Potter
E
L
(1963)
Amer.
J.
Obstet.
Gynec.
87,
566
Ueno
S,
Suzuki
K
&
Yamazawa
K
(1959)
A
cta
genet.
(Basel)
9,
47
Velez-Orozco
A
C
(1961)Bol.
Inst.
Estud.
mid.
biol.
(Mix.)
19,41
Wharton
B,
Edwards
J
H
&
Cameron
A
H
(1968)
J.
Obstet.
Gynae.
Brit.
Cwlth
(in
press)
Mr
J
V
O'Sullivan
(City
of
London
Maternity
Hospital,
London)
The
incidence
of
multiple
pregnancy
has
been
calculated
in
millions
of
deliveries;
it
varies
in
different
continents
and
different
races.
Among
Europeans
the
incidence
is:
twins,
one
in
86
births;
triplets,
one
in
862;
quadruplets,
one
in
863;
quintuplets,
one
in
50
million.
Sextuplets,
septuplets
and
even
octuplets
have
been
reported
recently.
It
is
usually
stated
that
uniovular
twins
come
from
a
single
ovum,
fertilized
by
one
spermato-
zoon.
One
division
of
the
oocyte
takes
place
and
each
cell
then
develops
into
an
identical
twin
with
the
same
blood
group,
sex,
fingerprints,
&c.
As
I
understand
it,
each
species
has
a
set
number
of
chromosomes
which
are
even
in
number.
Man
has
46
chromosomes
which
are
reduced
to
23
by
a
reduction
division
in
the
ovum
in
preparation
for
fertilization
by
a
sperm
which
has
similarly
reduced
its
chromosomes
to
23.
Conjugation
of
these
two
cells
brings
the
number
back
to
46.
It
is
assumed
that
each
chromosome
has
a
set
number
of
genes
necessary
to
produce
a
perfect
human
being.
It
is
difficult
therefore
for
me
to
understand
9
Section
of
Obstetrics
and
Gynaecology
235
the
present
teaching
on
identical
twins
and
still
more
to
understand
how
identical
triplets
or
identical
quins
can
occur
on
the
accepted
theories.
I
think
some
other
mechanism
is
at
work.
Perhaps
some
women,
like
hens,
produce
double
yoke
and
triple
yoke
eggs
with
separate
nuclei
which
are
fertilized
by
three
sperms
-
this
would
be
a
simpler
explanation
to
me.
The
question
'Do
woman
produce
eggs
with
two
nuclei,
&c.'
must
be
settled.
Separate
ova
fertilized
by
separate
sperms
is
straightforward.
Multiple
pregnancies
are
usually
diagnosed
between
the
30th
and
32nd
weeks,
a
few
earlier
and
some
later.
A
family
history
of
twins
may
be
helpful.
Excessive
vomiting,
excessive
strim
and
too
rapid
an
increase
of
weight
before
20
weeks
sometimes
occur.
Later,
at
32
weeks,
two
heads
may
be
felt.
The
girth
may
be
36
to
40
inches
(91-101
cm);
two
foetal
hearts
counted
for
one
minute
by
two
experts
may
have
a
rate
difference
of
more
than
ten.
The
size
of
the
uterus
is
much
the
same
in
multiple
and
single
pregnancies
until
the
18th
to
20th
week.
At
the
20th
week,
in
uniovular
twins,
hydramnios
starts
and
is
such
that
at
24
weeks
the
height
of
the
fundus
may
be
30
or
32
weeks
in
size.
Sometimes
fibroids
and
large
ovarian
cysts
may
lead
to
errors.
X-rays
at
the
33rd
week
are
usually
necessary
to
confirm
multiple
pregnancy,
to
show
the
lie
and
to
exclude
conjoined
twins.
Abortion
is
said
to
be
more
frequent;
prema-
ture
labour
is
certainly
more
common:
50%
of
mothers
go
into
labour
before
the
38th
week;
16%
before
the
36th
week;
16%
go
over
the
expected
date,
usually
multipara
(these
should
be
induced
at
term
where
possible).
Toxemias
of
pregnancy
occur
in
about
25
%
of
multiple
pregnancies;
they
are
about
three
times
more
common
than
in
a
single
pregnancy.
Anemia
is
markedly
increased,
both
iron
deficiency
and
macrocytic
types.
Hydramnios
occurs
in
single
pregnancies
in
0
5
%
of
cases,
and
in
8
%
of
multiple
pregnancies.
Hydramnios
contributes
to
malpresentation
and
post-partum
hemorrhage.
Ante-partum
haemorrhage
is
not
particularly
common;
post-partum
hemorrhage
is
very
common
and
very
dangerous
and
occurs
in
15
%
of
cases.
Antenatal
treatment
can
be
summed
up
as:
(1)
Control
of
hxemoglobin.
(2)
Rest
to
prevent
pre-
mature
labour.
(3)
Control
of
toxemia
by
rest,
diet,
&c.
(4)
Suitable
abdominal
support.
(5)
Control
of
acute
hydramnios,
by
repeated
paracentesis
together
with
the
application
of
Shirodka's
stitch.
The
faetal
loss
for
all
multiple
pregnancies
in
England
&
Wales
in
1959
was
8-9
%,
the
principal
cause
being
prematurity.
The
figures
are
gradually
being
improved.
For
some
years,
rest
in
hospital
for
up
to
four
weeks
has
been
recommended
to
reduce
the
incidence
of
premature
labour.
I
have
never
done
this
for
all
my
cases:
my
practice
has
been
to
admit
cases
of
hydramnios
as
soon
as
the
hydramnios
and
multiple
pregnancy
were
dia-
gnosed
or
patients
in
whom
the
cervix
was
found
dilated
to
one
finger
or
more
as
soon
as
twins
were
diagnosed
or
suspected.
An
analysis
of
twins
in
the
North
West
(Law
1967)
showed
that
routine
rest
in
hospital
did
not
influence
perinatal
mortality,
duration
of
pregnancy
or
the
birth
weight
of
the
babies.
All
multiple
pregnancies
should
be
delivered
in
hospital
because
of
the
danger
of
complications.
I
always
have
blood
available
and
usually
conduct
labour
in
multiple
pregnancy
under
a
physiological
oxytocin
drip,
2-5
units
in
a
litre
of
50%
glucose
given
intravenously
at
30
drops
a
minute.
As
soon
as
the
first
twin
is
born
I
cut
the
cord
between
ligatures,
examine
to
confirm
that
the
second
twin
is
in
a
longitudinal
lie,
rupture
the
second
sac
of
membranes
quickly,
push
the
presenting
part
into
the
brim
firmly
and
allow
the
rest
of
the
delivery
to
be
normal.
The
mortality
of
the
second
twin
is
greater
than
the
first
for
various
reasons,
one
of
which
is
allowing
a
long
interval
between
the
births:
the
half
hour
usually
recommended
is
too
long.
I
interfere
or
use
instruments
only
when
indi-
cated
as
in
a
single
pregnancy,
get
the
placenta
out
quickly
by
the
Brandt
&
Andrews
method,
and
then
give
ergometrine
0-25
mg
intravenously
and
0-25
mg
intramuscularly.
The
best
anesthesia
is
epidural
as
it
allows
immediate
intervention
where
necessary
and
has
no
ill
effect
on
the
babies.
The
best
weight
for
twin
babies
is
5j
lb
(2,500
g);
they
seem
to
do
better
than
the
heavier
ones.
REFERENCE
Law
R
G
(1967)
Standards
of
Obstetric
Care.
Report
of
the
North-
West
Metropolitan
Regional
Obstetric
Survey
1962-4.
Edinburgh
&
London

236
Proc.
roy.
Soc.
Med.
Volume
61
March
1968
Professor
W
J
Hamilton
(Charing
Cross
Hospital
Medical
School,
London)
said
that
it
was
much
more
likely
that
monozygotic
dichorionic
twins
would
arise
as
the
result
of
the
separation
of
the
first
two
blastomeres
rather
than,
as
Dr
Edwards
had
suggested,
at
the
morula
stage.
In
referring
to
Dr
Cameron's
contribution,
Professor
Hamilton
explained
that
his
own
practice
had
been
to
inject
Chromopaque
into
either
the
umbilical
artery
(or
arteries)
or
umbilical
veins;
the
placenta
had
then
been
X-rayed.
In
dizygotic
placentas
he
had
been
unable
to
detect
anastomoses
between
the
placental
vessels.
Anastomoses
had
been
readily
demonstrated
in
monozygotic
twins.
Professor
J
H
M
Pinkerton
(Queen's
University
of
Belfast,
Institute
of
Clinical
Science,
Belfast)
made
four
points:
(1)
Whilst
at
present
the
accurate
diagnosis
of
multiple
pregnancy
depended
upon
radiological
examination
it
was
likely
that
ultrasonic
tech-
niques
would
replace
radiology
for
this
purpose
in
the
future;
by
this
means
accurate
diagnosis
could
be
made
at
a
very
much
earlier
stage
of
pregnancy
without
radioactive
hazard.
(2)
There
was
as
little
place
for
domiciliary
mid-
wifery
as
for
domiciliary
surgery;
whilst
not
everyone
would
agree
with
this,
surely
even
the
most
sanguine
would
not
knowingly
risk
a
multiple
birth
outside
a
fully
equipped
hospital.
(3)
Prematurity
remained
a
very
real
danger
to
twins;
it
could
be
readily
forestalled
by
examining
the
cervix
from
the
24th
week
onwards
at
two-
weekly
intervals
and
admitting
the
patient
who
showed
progressive
dilatation.
(4)
There
was
nothing
to
be
gained
and
everything
to
be
lost
by
permitting
twins
to
remain
in
utero
beyond
40
weeks.
The
following
paper
was
also
read:
Results
of
the
Perinatal
Survey
Miss
Josephine
Barnes
and
Dr
Eve
Alberman
(National
Birthday
Trust
Fund)
[To
be
published
in
the
Second
Report
of
the
Perinatal
Mortality
Survey]
10
