Journal of Case Reports and Images in Obstetrics and Gynecology, Vol. 4, 2018.
J Case Rep Images Obstet Gynecol 2018;4:100042Z08SF2018.
www.edoriumjournals.com/case-reports/jcrog
Fischbein SJ 1
CASE REPORT OPEN ACCESS
A maneuver for head entanglement in term breech/vertex
twin labor
Stuart J. Fischbein
ABSTRACT
Whether planned or precipitous, some women
will present in advanced labor with a breech
first twin. We present a rare case of interlocking
heads in a woman with a term breech/vertex
pregnancy who strongly desired a vaginal birth.
A simple vaginal maneuver is described that led
to safe delivery of both twins.
Keywords: Breech, Complication, Inter-locking,
Twin
How to cite this article
Fischbein SJ. A maneuver for head entanglement in
term breech/vertex twin labor. J Case Rep Images
Obstet Gynecol 2018;4:100042Z08SF2018.
Article ID: 100042Z08SF2018
*********
doi: 10.5348/100042Z08SF2018CR
INTRODUCTION
When a first twin presents as breech a cesarean
section is generally recommended [1]. When twin A is
breech and twin B is vertex there is the concern for the
Stuart J. Fischbein
Affiliations: Birthing Instincts, Inc. 10309 Santa Monica
Blvd, Los Angeles, CA 90025, USA.
Corresponding Author: Stuart J. Fischbein, M.D., FACOG,
Birthing Instincts, Inc. 10309 Santa Monica Blvd, Los An-
geles, CA 90025, USA; Email: [email protected]
Received: 05 December 2018
Accepted: 16 December 2018
Published: 31 December 2018
rare complication of interlocking heads [2]. There is also
evidence that supports the vaginal delivery of breech
first twins and confirms the rarity of this complication
[3]. As with all aspects of pregnancy and labor, informed
consent is an integral part of the process. Mode of
delivery will often depend on the desire of the mother
in conjunction with the resources available to her. The
will and expertise to assist women with singleton or
twin breech birth, either A or B, is rapidly diminishing
leading to increasing cesarean rates for all breech and
twin births.
We present a case of diamniotic-dichorionic twins in
which twin A presented as complete breech and twin B
as vertex at 37 6/7 weeks. Descent of twin A arrested in
left sacrum transverse position with the feet and lower
body protruding. A diagnosis of head entanglement
was suspected and confirmed by vaginal exploration. A
fulcrum-like maneuver using the left hand internally
to elevate twin B’s head while freeing twin A led to
subsequent vaginal delivery of both twins.
Vaginal birth of many twin pregnancies is a reasonable
and evidence supported option. Fetal head entanglement
is a rare complication of breech/vertex twin births. For
women who choose to labor or present precipitously with
a breech first twin we present a successful maneuver for
resolving head entanglement.
CASE REPORT
A 32-year-old gravid 1, para 0 woman presented with
a diamniotic-dichorionic pregnancy by intrauterine
insemination for prenatal care at 11 weeks gestation.
There was no other pregnancy or health concerns.
Non-Invasive Prenatal Testing (NIPT and structural
ultrasound at 20 weeks were both normal. Babies were
concordant throughout. From approximately 26 weeks
on twin A was on maternal left and remained in complete
breech position. Twin B, on maternal right, was also in
breech position until 36 weeks at which point it became
vertex. Twin B was noted to have a dolicocephalic head
shape early on. During limited ultrasounds at 36 1/7 and
37 2/7 weeks it was determined that twin B’s head was
slightly lower in the pelvis than twin A’s head. There
was normal fluid and concordant growth. The mother
strongly desired a vaginal birth and was well informed
CASE REPORT PEER REVIEWED | OPEN ACCESS
Journal of Case Reports and Images in Obstetrics and Gynecology, Vol. 4, 2018.
J Case Rep Images Obstet Gynecol 2018;4:100042Z08SF2018.
www.edoriumjournals.com/case-reports/jcrog
Fischbein SJ 2
in all her options, preferred to wait for labor to arrive
and see how labor progressed.
In the early morning hours labor began becoming
active around noon. A vaginal exam at 1:15PM confirmed
complete breech at 5-6cm/100%/0 station and intact
membranes. By 4:55PM she was completely dilated with
bulging membranes. She was feeling an urge to push with
rectal pressure and began the second stage at 5:10PM.
Pushing was initiated on hands and knees. After about
40 minutes she changes to a semi-reclined position
due to fatigue on her arms and shoulders. At 5:50PM
the feet were seen to protrude from the introitus still
inside an intact sac. Contractions continued every 2 to 3
minutes and the Fetal Heart Rate (FHR) of both babies
via intermittent monitoring remained in the normal
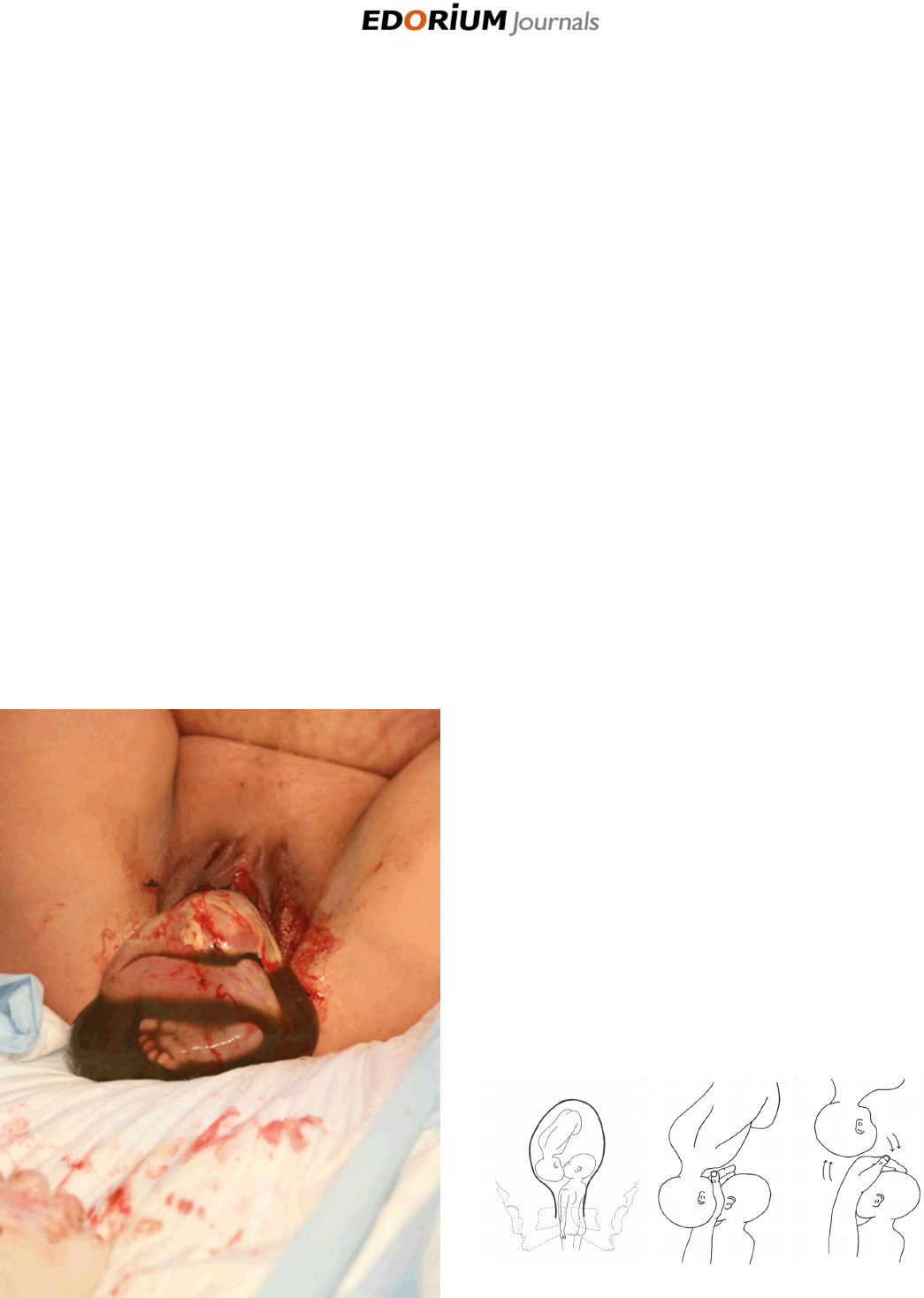
range without decelerations. By 6:09PM the legs and
rump had appeared still inside the intact amniotic sac
(Figure 1). There was good tone and capillary filling. At
6:12, the membranes were artificially ruptured releasing
watery meconium stained fluid. Twin A did not descend
any further and remained in the left sacrum transverse
position. Attempts at rotation (Loveset maneuver) were
unsuccessful in achieving any descent. The arms were
then swept down over the chest without much resistance
but still no descent and the head of twin B was evident
in the right lower quadrant. Abdominal manipulation
attempting to elevate twin B was unsuccessful in shifting
the positions. A diagnosis of head entanglement was made
(Figure 2A). The practitioner’s left hand was inserted up
along twin A’s body cupping its head in the palm while
using the back of the hand to elevate twin B’s head out of
the pelvis in a fulcrum like manner (Figure 2B-C). This
immediately freed twin A, who was then delivered easily
with use of the Mauriceau–Smellie–Veit maneuver at
6:15PM weighing 5 pounds 10 ounces with Apgar scores
of 7 & 9.
Prior to delivery of twin A the FHR of twin B was 160
with good variability. Three minutes post-delivery of twin
A the FHR of twin B was at 80-90bpm and vaginal exam
confirmed a cephalic presentation at -1 station. At 6:19
the membranes were artificially ruptured releasing clear
fluid. Mother was able to push twin B to +2 station but
baby was in the direct occiput posterior (OP) position
and FHR remained in the 90s. Uterine contractions had
diminished at this point and maternal pushing remained
ineffective. Low Tucker-McLane forceps were applied
with delivery of twin B, direct OP at 6:22PM. Apgar scores
were also 7 & 9 and the weight was 6 pounds 1 ounce. A
second degree laceration was noted and repaired.
DISCUSSION
In our case report we describe a well-informed woman
and her partner aware of the possibility of interlocked
or entangled heads but the rarity of this complication
made it a minor consideration. To insist, by coercion or
skewed counseling on a cesarean section for such a rare
occurrence against the wishes of the mother would not be
sound ethical practice. Labor progressed normally and
there was a normal second stage for twin A until descent
arrested. Breech delivery is facilitated on all fours and
shortens the second stage and expands the pelvis [4]. That
was evident here although the mother’s arms and legs got
tired and she had to switch to a semi-reclining position.
We do not think the position change contributed to the
head entanglement. More likely twin B’s dolicocephaly
prevented twin A’s head from passing by and both heads
descended in tandem. When descent and rotation of
a breech baby arrests it may be a signal the baby needs
assistance. The ineffectiveness of the usual maneuvers
Figure 1: Twin a still in caul remains left sacrum transverse.
Figure 2: (A) Entangled fetal heads result in arrest of descent for
Twin A. (B)Practitioner inserts hand vaginally. (C) Fulcrum-like
maneuver elevates Twin B releasing obstruction.

Journal of Case Reports and Images in Obstetrics and Gynecology, Vol. 4, 2018.
J Case Rep Images Obstet Gynecol 2018;4:100042Z08SF2018.
www.edoriumjournals.com/case-reports/jcrog
Fischbein SJ 3
to deliver twin A and the antenatal knowledge of the
position and shape of the head of twin B facilitated the
diagnosis of head entanglement. Intrapartum ultrasound
may assist if the diagnosis is in question but may consume
valuable time if not readily available. We present a novel
vaginal maneuver to elevate the head of the second twin
and facilitate passage of the breech twin. Using the back
of the hand to elevate the vertex of twin B while gently
cupping the head of twin A in a fulcrum-like fashion you
can release the obstruction and successfully complete the
vaginal breech delivery. If twin B is on mother’s right you
would use your left hand. If twin B is on the mother’s left
the practitioner would use the right hand.
The frequency of twin pregnancy in the U.S. in 2009
is about 1 in 30 pregnancies [5]. Vertex/vertex accounted
for 44%. Vertex/breech presentation occurred in 27%,
while breech/breech and breech/vertex occurred in 13%
each [6]. There is ongoing discussion about the best way
for term twins to deliver [7, 8, 9]. But no matter what the
studies may conclude the science is uncertain and women
may choose to exercise their right of informed consent
and refusal to choose any alternative. There is enough
evidence in the literature to support, as reasonable, the
choice of attempting vaginal birth with breech first twins.
When time is of the essence, use of stilled hands may
provide resolution before resorting to a surgical approach.
CONCLUSION
While no one has expertise in head entanglement
resolution, the skills acquired from hands on training
in breech delivery assist the practitioner with the spatial
relationships useful for problem solving in a highly
intense setting. We encourage the re-teaching of breech
and twin skills for just those rare moments such as this.
REFERENCES
1. Committee on practice bulletins—obstetrics; Society
for maternal–fetal medicine. Practice bulletin
no. 169: Multifetal gestations: Twin, triplet, and
higher-order multifetal pregnancies. Obstet Gynecol
2016;128(4):e131–46.
2. Borah T, Das A. Locked Twins: A Rarity. Ann Med
Health Sci Res 2012;2(2):204–5.
3. Blickstein I, Goldman RD, Kupferminc M. Delivery of
breech first twins: A multicenter retrospective study.
Obstet Gynecol 2000;95(1):37–42.
4. Louwen F, Daviss BA, Johnson KC, Reitter A. Does
breech delivery in an upright position instead of on
the back improve outcomes and avoid cesareans? Int
J Gynaecol Obstet 2017;136(2):151–61.
5. Martin JA, Hamilton BE, Osterman MJ. Three
decades of twin births in the United States, 1980–
2009. NCHS Data Brief 2012;(80):1–8.
6. Nnatu S. Presentation in twin pregnancy. Journal of
Obstetrics and Gynaecology 2009;6(1):35–7.
7. Dong Y, Luo ZC, Yang ZJ, et al. Is cesarean delivery
preferable in twin pregnancies at >=36 weeks
gestation? PLoS One 2016;11(5):e0155692.
8. Barrett JF, Hannah ME, Hutton EK, et al. A randomized
trial of planned cesarean or vaginal delivery for twin
pregnancy. N Engl J Med 2013;369(14):1295–305.
9. Steins Bisschop CN, Vogelvang TE, May AM,
Schuitemaker NW. Mode of delivery in non-cephalic
presenting twins: A systematic review. Arch Gynecol
Obstet 2012;286(1):237–47.
*********
Author Contributions
Stuart J. Fischbein – Substantial contributions to
conception and design, Acquisition of data, Analysis
and interpretation of data, Drafting the article, Revising
it critically for important intellectual content, Final
approval of the version to be published
Guarantor of Submission
The corresponding author is the guarantor of submission.
Source of Support
None.
Consent Statement
Written informed consent was obtained from the patient
for publication of this case report.
Conflict of Interest
Author declares no conflict of interest.
Data Availability
All relevant data are within the paper and its Supporting
Information files.
Copyright
© 2018 Stuart J. Fischbein et al. This article is distributed
under the terms of Creative Commons Attribution
License which permits unrestricted use, distribution
and reproduction in any medium provided the original
author(s) and original publisher are properly credited.
Please see the copyright policy on the journal website for
more information.
Journal of Case Reports and Images in Obstetrics and Gynecology, Vol. 4, 2018.
J Case Rep Images Obstet Gynecol 2018;4:100042Z08SF2018.
www.edoriumjournals.com/case-reports/jcrog
Fischbein SJ 4
Access full text article on
other devices
Access PDF of article on
other devices